Meta-analysis of the relationship between maternal adverse childhood experiences and offspring maladaptive social behaviors
-
摘要:
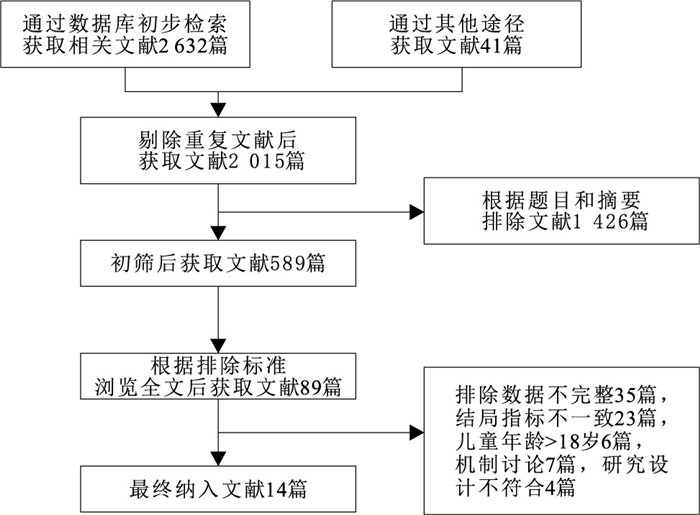
目的 分析母亲不良童年经历与儿童社会行为的相关性,为进一步开展母亲及儿童社会行为相关研究提供理论依据。 方法 检索建库至2025年5月中国知网(CNKI)、维普、万方、SinoMed、PubMed、Web of Science、Cochrane Library、Embase、SpringLink数据库中与母亲不良童年经历和儿童不良社会行为发展相关的研究。中文数据库通过3组关键词进行匹配检索:“孕产妇”“母亲”“女性”; “童年不良经历”“早年不良经历”“青少年不良经历”; “儿童”“青少年”“儿童行为”“儿童发展”“青少年行为”“内化行为”“外化行为”。英文数据库通过3组关键词进行检索:“Female”“Pregnant women”“Mothers”; “Adverse childhood experiences”“Adverse early childhood experiences”“Adverse experiences of adolescent”; “Child behavior”“Child development” “Adolescent behavior”“Internalized behaviors”“Externalized behaviors”。对筛选出的文献进行质量评价、资料提取,以比值比(OR)和置信区间(95%CI)为效应指标。采用State 16.0软件进行异质性检验、亚组分析、发表偏倚分析等。 结果 最终纳入14篇文献,共64 302对母子。Meta分析结果显示,母亲不良童年经历与儿童不良的内化行为(OR=1.75,95%CI=1.42~2.15)和外化行为(OR=1.82,95%CI=1.51~2.20)均呈正相关(P值均 < 0.01)。亚组分析结果显示,母亲不良童年经历与儿童不良的内化行为、外化行为在不同研究地区[内化行为:国内、国外OR值(95%CI)分别为2.03(1.49~2.76),1.55(1.19~2.03);外化行为:国内、国外OR值(95%CI)分别为2.41(1.52~3.82),1.65(1.36~2.01)]、研究方法[内化行为:队列研究、横断面研究OR值(95%CI)分别为1.64(1.34~2.00),1.85(1.30~2.65);外化行为:队列研究、横断面研究OR值(95%CI)分别为1.76(1.46~2.12),2.12(1.40~3.20)]、样本量[内化行为:≥4 000, < 4 000对OR值(95%CI)分别为1.69(1.13~2.55),1.77(1.41~2.24);外化行为:≥3 000, < 3 000对OR值(95%CI)分别为1.72(1.37~2.17),2.13(1.44~3.15)]等均呈正相关(P值均 < 0.05)。 结论 母亲不良童年经历与儿童不良内化行为、外化行为的发展均呈正相关,但该结果仍需要更多的研究继续验证。 Abstract:Objective To systematically evaluate the association between maternal adverse childhood experiences (ACEs) and offspring social behavior, so as to provide a theoretical basis for further research on intergenerational social behavioral development. Methods Relevant research literature about maternal ACEs and the development of children's maladaptive social behaviors were collected, from China National Knowledge Infrastructure (CNKI), VIP, Wanfang, SinoMed, PubMed, Web of Science, Cochrane Library, Embase and SpringLink databases, covering the period from the inception of each database to May 2025. The Chinese database matched and searched through three groups of keywords: "Pregnant women" "Mothers" and "Women"; "Bad childhood experience" "Bad early experience" and "Bad adolescent experience"; "Children" "Teenagers" "Children's behavior" "Children's development" "Teenagers' behavior" "Internalized behavior" and "Externalized behavior". The English database was searched by three groups of keywords: "Female" "Pregnant women" "Mothers"; "Adverse childhood experiences" "Adverse early childhood experiences" "Adverse experiences of adolescent"; "Child behavior" "Child development" "Adolescent behavior" "Internalized behaviors" "Externalized behaviors". The selected literature was evaluated for quality and data extraction, with OR and 95%CI as effect indicators. Stata 16.0 software was used for heterogeneity testing, subgroup analysis, and publication bias analysis. Results A total of 14 studies involving 64 302 mother-child pairs were included. The Meta-analysis results showed a significant correlation between maternal ACEs and both offspring maladaptive internalized behaviors (OR=1.75, 95%CI=1.42-2.15, P < 0.01) and externalized behaviors (OR=1.82, 95%CI=1.51-2.20, P < 0.01). The results of subgroup analyses showed that in different regions[internalized behaviors: domestic, foreign OR(95%CI)=2.03(1.49-2.76), 1.55(1.19-2.03); externalized behaviors: domestic, foreign OR(95%CI)=2.41(1.52-3.82), 1.65(1.36-2.01)], study type[internalized behaviors: cohort study, cross-sectional study OR(95%CI)=1.64(1.34-2.00), 1.85(1.30-2.65); externalized behaviors: cohort study, cross-sectional study OR(95%CI)=1.76(1.46-2.12), 2.12(1.40-3.20)], sample size [internalized behaviors: ≥4 000, < 4 000 pairs OR(95%CI)=1.69(1.13-2.55), 1.77(1.41-2.24); externalized behaviors: ≥3 000, < 3 000 pairs OR(95%CI)=1.72(1.37-2.17), 2.13(1.44-3.15)], there were significant and positive association between mothers' ACEs and children's internalizing and externalizing behaviors (all P < 0.05). Conclusion A substantial positive association exists between maternal ACEs and the development of offspring maladaptive internalized and externalized behaviors, but the result needs to be continued to be validated by more research. -
Key words:
- Mothers /
- Life change events /
- Social behavior /
- Meta-analysis /
- Mental health /
- Child
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 母亲不良童年经历与儿童不良社会行为关系纳入文献的基本信息
Table 1. Basic information of included literature on the relationship between maternal adverse childhood experiences and children's maladaptive social behavior
第一作者与年份 国家 研究方法 样本量/对 儿童社会心理类别 测量工具 儿童年龄/岁 OR值(95%CI) 文献质量评价 Moog(2023)[14] 美国 队列研究 3 954 内化问题 工具4 < 18 2.70(1.95~3.72) 高 自闭症 < 18 1.70(1.13~2.55) 多动症 < 18 2.09(1.63~2.67) McDonald(2019)[15] 加拿大 队列研究 3 000 多动/注意力不集中 工具4 3 1.50(1.16~1.94) 高 高程度身体攻击性 3 1.61(1.21~2.13) 焦虑/情绪障碍 3 1.46(1.06~2.02) 高水平分离焦虑 3 1.32(1.03~1.70) Wang(2022)[16] 中国 横断面研究 7 318 行为问题 工具3 4.43±0.98 2.91(2.45~3.45) 中 Zhang(2025)[17] 中国 横断面研究 3 672 抑郁 工具2 13.98±1.62 1.31(1.07~1.61) 高 Doi(2021)[18] 日本 横断面研究 9 390 儿童行为问题 工具7 < 18 2.04(1.64~2.44) 中 儿童抑郁症状 工具10 < 18 0.69(0.39~0.99) Moon(2021)[19] 韩国 横断面研究 461 注意力缺陷多动障碍 工具1 13.26±3.91 1.24(1.04~1.48) 中 Na(2021)[20] 韩国 横断面研究 156 创伤后应激障碍 工具1 16.58±1.47 3.01(1.24~7.31) 中 Luo(2023)[21] 中国 横断面研究 4 243 冲动-多动 工具3 4.60±1.00 2.24(1.29~3.88) 高 焦虑 4.60±1.00 2.46(1.30~4.46) Li(2024)[22] 中国 横断面研究 9 647 行为问题 工具7 5.1±0.9 2.39(1.95~2.94) 中 Hetherington(2020)[23] 加拿大 队列研究 2 909 内化行为 工具9 < 18 1.58(1.12~2.23) 中 外化行为 < 18 2.59(1.75~3.80) McConnell(2025)[24] 美国 队列研究 5 445 外化行为 工具5 4~14 1.50(1.25~1.80) 高 内化行为 4~14 1.50(1.23~1.81) 郭锋(2022)[25] 中国 横断面研究 3 655 自闭症 工具6 3~6 2.77(1.92~3.99) 中 李秋容(2024)[26] 中国 横断面研究 805 解决问题能力 工具8 3~5.6 3.80(1.20~12.00) 中 沟通能力 3~5.6 6.90(2.30~20.30) 粗大动作 3~5.6 3.80(1.50~9.70) 余伟强(2022)[27] 中国 横断面研究 9 647 情绪症状 工具7 5.1±0.9 3.09(2.28~4.18) 中 品行问题 5.1±0.9 2.18(1.70~2.80) 多动障碍 5.1±0.9 2.07(1.67~2.57) 同伴交往 5.1±0.9 1.26(1.08~1.47) 亲社会行为 5.1±0.9 1.37(1.12~1.67) 注:工具1~10分别为诊断预测量表(Predictive Scales, DPS),流行病学研究中心抑郁量表(Center for Epidemiological Studies Depression Scale, CES-D),康纳斯父母评分量表(48-Item Conners' Parent Rating Scale, CPRS-48),儿童行为量表(Child Behaviour Check List, CBCL),28项行为问题指数(28-Item Behavior Problem Index),克氏自闭症行为量表(Clancy Autism Behavior Scale, CABS),长处和困难问卷(Strength and Difficulties Questionnaire, SDQ),年龄与发育进程问卷-3(Ages and Stages Questionnaines-3, ASQ-3),儿童行为评估系统第二版(Behavior Assessment System for Children-Second Edition, BASC-2),抑郁障碍自评量表(Depression Self-rating Scale, DSRS)。 表 2 母亲不良童年经历与儿童内化行为、外化行为关系的亚组分析
Table 2. Subgroup analysis of the relationship between maternal adverse childhood experiences and children's internalizing and externalizing behaviors
亚组 选项 内化行为 外化行为 研究数量 OR值(95%CI) I2值/% P值 研究数量 OR值(95%CI) I2值/% P值 地区 国内 4 2.03(1.49~2.76) 86.15 < 0.01 3 2.41(1.52~3.82) 86.12 < 0.01 国外 6 1.55(1.19~2.03) 80.51 < 0.01 5 1.65(1.36~2.01) 74.46 < 0.01 研究方法 队列研究 4 1.64(1.34~2.00) 64.76 0.02 4 1.76(1.46~2.12) 60.04 0.04 横断面研究 6 1.85(1.30~2.65) 89.93 < 0.01 4 2.12(1.40~3.20) 90.62 < 0.01 样本量/对 ≥4 000/3 000 4 1.69(1.13~2.55) 88.18 < 0.01 4 1.72(1.37~2.17) 79.47 < 0.01 < 4 000/3 000 6 1.77(1.41~2.24) 74.38 < 0.01 4 2.13(1.44~3.15) 85.63 < 0.01 注: *P < 0.05,**P < 0.01;内化行为样本量以4 000对为分界点,外化行为以3 000对为分界点。 -
[1] DEIGHTON S, NEVILLE A, PUSCH D, et al. Biomarkers of adverse childhood experiences: a scoping review[J]. Psychiatry Res, 2018, 269: 719-732. doi: 10.1016/j.psychres.2018.08.097 [2] FELITTI V J, ANDA R F, NORDENBERG D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults the adverse childhood experiences (ACE) study[J]. Am J Prev Med, 1998, 14(4): 245-258. doi: 10.1016/S0749-3797(98)00017-8 [3] TZOUVARA V, KUPDERE P, WILSON K, et al. Adverse childhood-experiences, mental health, and social functioning: a scoping review of the literature[J]. Child Abuse Negl, 2023, 139: 106092. doi: 10.1016/j.chiabu.2023.106092 [4] ANDA R F, FELITTI V J, BREMNER J D, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology[J]. Eur Arch Psychiatry Clin Neurosci, 2006, 256(3): 174-186. doi: 10.1007/s00406-005-0624-4 [5] WEN D J, POH J S, NI S N, et al. Influences of prenatal and postnatal maternal depressionon amygdala volume andmicrostructure in young children[J]. Transl Psychiatry, 2017, 7(4): e1103. doi: 10.1038/tp.2017.74 [6] SAVIOS BEERS L A, HOLLO R E. Approaching the adolescent-headed family: a review of teen parenting[J]. Curr Probl Pediatr Adolesc Health Care, 2009, 39(9): 216-233. [7] HUNT T K A, SLACK K S, BERGER L M. Adverse childhood experiences and behavioral problems in middle childhood[J]. Child Abuse Negl, 2017, 67: 391-402. doi: 10.1016/j.chiabu.2016.11.005 [8] MCKELVEY L M, EDGE N C, MESMAN G R, et al. Adverse experiences in infancy and toddlerhood: relations to adaptive behavior and academic status in middle childhood[J]. Child Abuse Negl, 2018, 82: 168-177. doi: 10.1016/j.chiabu.2018.05.026 [9] GULENC A, BUTLER E, SARKADI A, et al. Paternal psychological distress, parenting, and child behaviour: a population based, cross-sectional study[J]. Child Care Health Dev, 2018, 44(6): 892-900. doi: 10.1111/cch.12607 [10] MCRAE E M, STOPPELBEIN L, O'KELLEY S E, et al. Predicting child behavior: a comparative analysis between autism spectrum disorder and attention deficit/hyperactivity disorder[J]. J Child Fam Stud, 2019, 28(3): 668-683. doi: 10.1007/s10826-018-1299-6 [11] NIKSTAT A, BEAM C R, RIEMANN R. Gene-environment interplay in internalizing problem behavior[J]. Dev Psychol, 2023, 59(8): 1470-1483. doi: 10.1037/dev0001567 [12] 顾莺, 张慧文, 周英凤, 等. JBI循证卫生保健中心关于不同类型研究的质量评价工具: 系统评价的方法学质量评价[J]. 护士进修杂志, 2018, 33(8): 701-703.GU Y, ZHANG H W, ZHOU Y F, et al. JBI evidence-based health center's quality assessment tool for different types of research: the quality evaluation of diagnostic and economic evaluation[J]. J Nurses Train, 2018, 33(8): 701-703. (in Chinese) [13] 曾宪涛, 刘慧, 陈曦, 等. Meta分析系列之四: 观察性研究的质量评价工具[J]. 中国循证心血管医学杂志, 2012, 4(4): 297-299.ZENG X T, LIU H, CHEN X, et al. Meta-analysis series Ⅳ: quality evaluation tools for observational research[J]. Chin J Evid Based Cardiovasc Med, 2012, 4(4): 297-299. (in Chinese) [14] MOOG N K, CUMMINGS P D, JACKSON K L, et al. Intergenerational transmission of the effects of maternal exposure to childhood maltreatment in the USA: a retrospective cohort study[J]. Lancet Public Health, 2023, 8(3): e226-e237. doi: 10.1016/S2468-2667(23)00025-7 [15] MCDONALD S W, MADIGAN S, RACINE N, et al. Maternal adverse childhood experiences, mental health, and child behaviour at age 3: the all our families community cohort study[J]. Prev Med, 2019, 118: 286-294. doi: 10.1016/j.ypmed.2018.11.013 [16] WANG X, YIN G, GUO F, et al. Associations of maternal adverse childhood experiences with behavioral problems in preschool children[J]. J Interpers Violence, 2022, 37(21/22): NP20311-NP20330. [17] ZHANG Y, HE Y, XUE Z, et al. Association between maternal exposure to cumulative childhood trauma and offspring childhood trauma and depressive symptoms among Chinese adolescents[J]. BMC Public Health, 2025, 25(1): 1795. doi: 10.1186/s12889-025-22613-7 [18] DOIS, FUJIWARA T, ISUMI A. Association between maternal adverse childhood experiences and mental health problems in offspring: an intergenerational study[J]. Dev Psychopathol, 2021, 33(3): 1041-1058. doi: 10.1017/S0954579420000334 [19] MOON D S, BONG S J, KIM B N, et al. Association between maternal adverse childhood experiences and attention-deficit/hyperactivity disorder in the offspring: the mediating role of antepartum health risks[J]. Soa Chongsonyon Chongsin Uihak, 2021, 32(1): 28-34. [20] NA M C, KIM M D, PARK J H, et al. Association between maternal adverse childhood experiences and risk of post-traumatic stress disorder in the offspring[J]. Soa Chongsonyon Chongsin Uihak, 2021, 32(2): 63-70. [21] LUO S, CHEN D, LI C, et al. Maternal adverse childhood experiences and behavioral problems in preschool offspring: the mediation role of parenting styles[J]. Child Adolesc Psychiatry Ment Health, 2023, 17(1): 95. doi: 10.1186/s13034-023-00646-3 [22] LI R, XIAO W, WU J, et al. Patterns of maternal adverse childhood experiences and the intergenerational association of preschool children's emotional and behavioral problems[J]. Front Psychiatry, 2024, 15: 1431475. doi: 10.3389/fpsyt.2024.1431475 [23] HETHERINGTON E, RACINE N, MADIGAN S, et al. Relative contribution of maternal adverse childhood experiences to understanding children's externalizing and internalizing behaviours at age 5: findings from the All Our Families cohort[J]. CMAJ Open, 2020, 8(2): E352-E359. doi: 10.9778/cmajo.20190149 [24] MCCONNELL K, GLEASON J, SHENASSA E. Association between maternal adverse childhood experiences and offspring internalizing and externalizing behavior[J]. Obstet Gynecol, 2025, 146(2): 267-273. doi: 10.1097/AOG.0000000000005946 [25] 郭锋, 汪小燕, 殷刚柱, 等. 母亲童年期不良经历与学龄前儿童自闭症行为的关联[J]. 中国学校卫生, 2022, 43(8): 1143-1147. doi: 10.16835/j.cnki.1000-9817.2022.08.006GUO F, WANG X Y, YIN G Z, et al. Relationships between maternal adverse childhood experiences and autistic behaviors in preschool children[J]. Chin J Sch Health, 2022, 43(8): 1143-1147. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2022.08.006 [26] 李秋容, 李金秀, 吕小平, 等. 母亲童年期不良经历与儿童神经心理发育的关联研究[J]. 广西医科大学学报, 2024, 41(2): 294-301.LI Q R, LI J X, LÜ X P, et al. Association between maternal adverse childhood experiences and children's neuropsychological development[J]. J Guangxi Med Univ, 2024, 41(2): 294-301. (in Chinese) [27] 余伟强, 李若瑜, 黄永玲, 等. 母亲童年期不良经历与学龄前儿童情绪行为问题的关联[J]. 中国学校卫生, 2022, 43(8): 1130-1133, 1138. doi: 10.16835/j.cnki.1000-9817.2022.08.003YU W Q, LI R Y, HUANG Y L, et al. Relationship between maternal adverse childhood experiences and preschool children's emotional and behavioral problems[J]. Chin J Sch Health, 2022, 43(8): 1130-1133, 1138. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2022.08.003 [28] EDWARDS R C, HANS S L. Infant risk factors associated with internalizing, externalizing, and co-occurring behavior problems in young children[J]. Dev Psychol, 2015, 51(4): 489-499. doi: 10.1037/a0038800 [29] DITTRICH K, BERMPOHL F, KLUCZNIOK D, et al. Alterations of empathy in mothers with a history of early life maltreatment, depression, and borderline personality disorder and their effects on child psychopathology[J]. Psychol Med, 2020, 50(7): 1182-1190. doi: 10.1017/S0033291719001107 [30] AZEREDO C M, SANTOS I S, BARROS A J D, et al. Maternal depression and bullying victimization among adolescents: results from the 2004 Pelotas cohort study[J]. Depress Anxiety, 2017, 34(10): 897-907. doi: 10.1002/da.22662 [31] WEISSMAN M M, WICKRAMARATNE P, PILOWSKY D J, et al. The effects on children of depressed mothers' remission and relapse over 9 months[J]. Psychol Med, 2014, 44(13): 2811-2824. doi: 10.1017/S003329171400021X [32] TURNER K, ZAMBRELLI E, BASSANESE G, et al. Effects of postpartum depression on the behaviour of children born to mothers with epilepsy[J]. Seizure, 2019, 73: 31-38. doi: 10.1016/j.seizure.2019.10.018 [33] MARTINEZ-TORTEYA C, DAYTON C J, BEEGHLY M, et al. Maternal parenting predicts infant biobehavioral regulation among women with a history of childhood maltreatment[J]. Dev Psychopathol, 2014, 26(2): 379-392. doi: 10.1017/S0954579414000017 [34] ROTH M C, HUMPHREYS K L, KING L S, et al. Attachment security in pregnancy mediates the association between maternal childhood maltreatment and emotional and behavioral problems in offspring[J]. Child Psychiatry Hum Dev, 2021, 52(5): 966-977. doi: 10.1007/s10578-020-01073-7 [35] WIGGINS J L, MITCHELL C, HYDE L W, et al. Identifying early pathways of risk and resilience: the codevelopment of internalizing and externalizing symptoms and the role of harsh parenting[J]. Dev Psychopathol, 2015, 27(4 Pt 1): 1295-1312. [36] HALLIGAN S L, MURRAY L, MARTINS C, et al. Maternal depression and psychiatric outcomes in adolescent offspring: a 13-year longitudinal study[J]. J Affect Disord, 2007, 97(1/2/3): 145-154. [37] LINDE-KRIEGER L, YATES T M. Mothers' history of child sexual abuse and child behavior problems: the mediating role of mothers' helpless state of mind[J]. Child Maltreat, 2018, 23(4): 376-386. doi: 10.1177/1077559518775536 [38] YOON Y, CEDERBAUM J A, MENNEN F E, et al. Linkage between teen mother's childhood adversity and externalizing behaviors in their children at age 11: three aspects of parenting[J]. Child Abuse Negl, 2019, 88: 326-336. doi: 10.1016/j.chiabu.2018.12.005 [39] BERTHELON M, CONTRERAS D, KRUGER D, et al. Harsh parenting during early childhood and child development[J]. Econ Hum Biol, 2020, 36: 100831. doi: 10.1016/j.ehb.2019.100831 -





 下载:
下载: