Stakeholder analysis of prevention and control of obesity among middle school students
-
摘要:
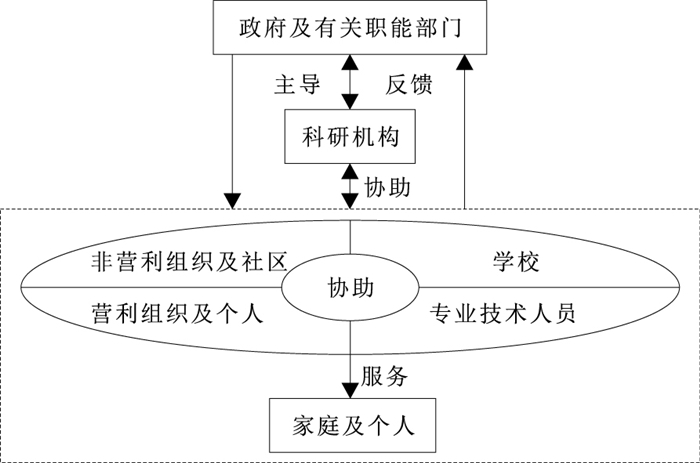
目的 识别初中生肥胖防控利益相关者并分析其参与初中生肥胖防控的动机与利益诉求, 为促进利益相关者有效参与初中生肥胖防控提供建设性意见。 方法 通过文献分析结合17名儿童青少年肥胖防控专家函询结果确定利益相关者及其分类。采用方便抽样方法, 于2023年12月至2024年1月通过与11名初中生肥胖防控有关工作人员面对面访谈, 并与48名学生及家长进行专题小组访谈, 采用主题分析法获取利益相关者参与肥胖防控的动机与利益诉求。 结果 共识别政府及有关职能部门、非营利组织及社区、营利组织及个人、学校、专业技术人员、家庭及个人、科研机构7个方面29类利益相关者, 其中28类均为确定型利益相关者。利益相关者之间存在管理、协助、服务共3类关系。阻碍利益相关者合作的因素可归纳为专项政策不完善且未形成长效合作机制、考核机制存在缺陷及利益冲突、物质资源不足、不良健康观念。受访者提出在合作形式方面可成立青少年肥胖防控专题小组; 在合作内容方面制定并签署肥胖防控责任书, 加大对营利组织的监管力度、肥胖防控的宣传力度和财政支持力度。 结论 初中生肥胖防控可参照利益相关者角色和关系组建合作联盟, 通过利益整合、目标整合和精神整合的策略调和感知利益冲突, 提高项目的可行性、参与度和可持续性。 Abstract:Objective To identify the stakeholders of prevention and control of obesity among middle school students and analyze their motivations and interest demands for participation, in order to provide constructive recommendations for facilitating their effective engagement of stakeholders in prevention and control of obesity among middle school students. Methods Stakeholders and their types were identified through a combination of literature analysis and consultation with 17 experts in children and adolescents for prevention and control of obesity. From December 2023 to January 2024, by applying convenience sampling, face-to-face semi-structured interviews were conducted with 11 individuals engaged in prevention and control of obesity for middle school students and focus group interviews were conducted with 48 students and parents. Thematic analysis was employed to obtain motivations and interest demands for stakeholder involvement in prevention and control of obesity. Results A total of 29 subcategories within 7 major categories of stakeholders were identified, including government and relevant functional departments, non-profit organizations and communities, for-profit organizations and individuals, schools, professional and technical personnel, families and individuals, and scientific research institutions, with 28 subcategories being confirmed stakeholders. Among these stakeholders, there were 3 types of cooperative relationships: management, cooperation, and service. There were some factors hindering cooperation among stakeholders including imperfections in specialized policies and lack of long-term cooperative mechanisms, flaws and interest conflicts in the evaluation system, insufficiency of material resources, and poor health values. In response to these challenges, interviewees proposed to convene a working group for the prevention and control of adolescent obesity. They also suggested making a contract of responsibility, strengthening supervision over for-profit organizations, enhancing advocating efforts for prevention and control of obesity, and increasing financial support. Conclusions The prevention and control of obesity for middle school students can be facilitated by forming a collaborative alliance based on the roles and relationships of stakeholders identified in the present study. Perceived conflicts of interest among stakeholders can be reconciled by employing strategies of interest integration, goal alignment, and spiritual integration, to enhance the feasibility, participation and sustainability of obesity intervention. -
Key words:
- Obesity /
- Preventive health services /
- Health personnel /
- Organization and administration
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 初中生肥胖防控利益相关者分类
Table 1. Classification of stakeholders for prevention and control of obesity among middle school students
类别 利益相关者 权力性 合法性 紧迫性 总分 类型 政府及有关职能部门 教育局 4.71 4.53 4.65 4.63 确定型 卫生健康委员会 4.41 4.88 4.53 4.61 确定型 疾病预防控制中心 4.12 4.71 4.53 4.45 确定型 体育局 3.76 4.35 4.35 4.16 确定型 市场监督管理局 2.71 3.53 3.41 3.22 确定型 社区街道办事处 2.65 3.41 3.29 3.12 确定型 非营利组织及社区 健康类社会团体,如食品安全与营养学会 3.47 3.59 3.76 3.61 确定型 社区卫生服务中心 3.18 3.82 3.24 3.41 确定型 体育类社会团体,如体育运动协会 3.41 3.47 3.29 3.39 确定型 基金会,如青少年发展基金会 2.94 3.47 3.47 3.29 确定型 青少年发展类社会团体,如共青团 3.12 3.47 3.29 3.29 确定型 社区居委会 2.65 3.35 2.94 2.98 预期型 营利组织及个人 体育场馆及健身服务经营者 3.18 3.35 3.24 3.25 确定型 食品生产、加工、销售经营者,餐饮服务经营者 3.18 3.29 3.18 3.22 确定型 学校 校领导 4.65 4.53 4.24 4.47 确定型 校医 4.06 4.47 4.24 4.25 确定型 专任教师 3.88 4.35 4.06 4.10 确定型 家长委员会 3.76 4.06 3.94 3.92 确定型 食堂工作人员 3.47 4.06 3.88 3.80 确定型 专业技术人员 营养指导员 4.18 4.65 4.12 4.31 确定型 医疗卫生服务人员 4.18 4.41 4.06 4.22 确定型 社会体育指导员 3.82 4.18 3.88 3.96 确定型 家庭教育指导师 3.65 4.06 3.76 3.82 确定型 心理健康工作人员 3.53 3.82 3.88 3.75 确定型 家庭及个人 学生 4.53 4.76 4.47 4.59 确定型 家长及照护者 4.59 4.65 4.47 4.57 确定型 科研机构 公共卫生科研机构 4.18 4.29 4.41 4.29 确定型 运动健康研究机构 4.00 4.24 4.12 4.12 确定型 儿童青少年发展研究机构 4.00 4.06 4.18 4.08 确定型 -
[1] LOBSTEIN T, JACKSON-LEACH R, MOODIE M L, et al. Child and adolescent obesity: part of a bigger picture[J]. Lancet, 2015, 385(9986): 2510-2520. doi: 10.1016/S0140-6736(14)61746-3 [2] KARNIK S, KANEKAR A. Childhood obesity: a global public health crisis[J]. Int J Prev Med, 2012, 3(1): 1-7. [3] 原晨晨, 薛琨, 郭红卫. 全球儿童超重肥胖的流行现状和影响因素[J]. 卫生研究, 2020, 49(3): 506-510.YUAN C C, XUE K, GUO H W. Global prevalence and influencing factors of overweight and obesity in children[J]. J Hyg Res, 2020, 49(3): 506-510. (in Chinese) [4] 王军利, 项立敏, 张松奎, 等. 儿童青少年超重与肥胖的成因及社会网络干预[J]. 上海体育学院学报, 2019, 43(5): 30-40.WANG J L, XIANG L M, ZHANG S K, et al. Factors and social network interventions of overweight and obesity in children and adolescents[J]. J Shanghai Sport Univ, 2019, 43(5): 30-40. (in Chinese) [5] BLEICH S N, VERCAMMEN K A, ZATZ L Y, et al. Interventions to prevent global childhood overweight and obesity: a systematic review[J]. Lancet Diabetes Endocrinol, 2018, 6(4): 332-346. doi: 10.1016/S2213-8587(17)30358-3 [6] 王海俊, 严诗钰. 儿童青少年肥胖干预研究需开展依从性评价[J]. 中国学校卫生, 2023, 44(4): 481-484. doi: 10.16835/j.cnki.1000-9817.2023.04.001 WANG H J, YAN S Y. Obesity intervention studies in children and adolescents need compliance evaluation[J]. Chin J Sch Health, 2023, 44(4): 481-484. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2023.04.001 [7] FREEMAN R E. Strategic management: a stakeholder approach[M]. Boston: Pitman, 1984. [8] ISRAEL B A, SCHULZ A J, PARKER E A, et al. Critical issues in developing and following community-based participatory research principles[M]//MINKLER M, WALLERSTEIN N. Community-based participatory research for health. San Francisco, CA: Jossey-Bass, 2008: 47-62. [9] KORN A R, APPEL J, HAMMOND R A, et al. Validation and refinement of the stakeholder-driven community diffusion survey for childhood obesity prevention[J]. Implement Sci, 2021, 16(1): 1-13. doi: 10.1186/s13012-020-01068-x [10] BUTTIVANT H, KNAI C. Improving food provision in child care in England: a stakeholder analysis[J]. Public Health Nutr, 2012, 15(3): 554-560. doi: 10.1017/S1368980011001704 [11] CALANCIE L, NAPPI D, APPEL J, et al. Implementing and evaluating a stakeholder-driven community diffusion: informed early childhood intervention to prevent obesity, Cuyahoga County, Ohio, 2018-2020[J]. Prev Chronic Dis, 2022, 19: E03. [12] SCHILLER C, WINTERS M, HANSON H M, et al. A framework for stakeholder identification in concept mapping and health research: a novel process and its application to older adult mobility and the built environment[J]. BMC Public Health, 2013, 13(1): 1-9. doi: 10.1186/1471-2458-13-1 [13] HART G. The five W's: an old tool for the new task of audience analysis[J]. Tech Commun, 1996, 43(2): 139-145. [14] PAN Z, KOSICKI G. Framing analysis: an approach to news discourse[J]. Polit Commun, 1993, 10: 55-75. doi: 10.1080/10584609.1993.9962963 [15] MITCHELL R K, AGLE B R, WOOD D J. Toward a theory of stakeholder identification and salience: defining the principle of who and what really counts[J]. Acad Manage Rev, 1997, 22(4): 853. doi: 10.2307/259247 [16] 张浩为, 梁立波, 孙宏, 等. 公立医院薪酬体系利益相关者分析[J]. 中国医院管理, 2017, 37(10): 30-32.ZHANG H W, LIANG L B, SUN H, et al. Analysis of the salary system stakeholders in public hospitals[J]. Chin Hosp Manage, 2017, 37(10): 30-32. (in Chinese) [17] 中华人民共和国国家卫生健康委办公厅, 中华人民共和国教育部办公厅, 国家市场监督管理总局办公厅, 等. 关于印发儿童青少年肥胖防控实施方案的通知[J]. 中华人民共和国教育部公报, 2020(11): 18-21.General Office of the National Health Commission of the PRC, General Office of the Ministry of Education of the PRC, General Office of the State Administration for Market Regulation, et al. Notice of issuance of the implementation plan for obesity control in children and adolescents[J]. Bull Minist Educ PRC, 2020(11): 18-21. (in Chinese) [18] 陈莹莹, 鄢雪松, 邹青海. "双减"政策背景下远程青少年体质健康教育扶贫的实践困囿及突围路径: 基于利益相关者分析[J]. 体育科技文献通报, 2023, 31(4): 119-123.CHEN Y Y, YAN X S, ZOU Q H. Practical difficulties and solutions of poverty alleviation through remote physical health education for adolescents under the background of Double Reduction policy: based on stakeholder analysis[J]. Bull Sport Sci Technol, 2023, 31(4): 119-123. (in Chinese) [19] 陈亮. 冲突与均衡: 社区体医融合健康服务的利益相关者共治研究[J]. 中国卫生事业管理, 2022, 39(10): 736-741, 800.CHEN L. Conflict and balance: a stakeholder co-governance study of community sports and medicine integrated health services[J]. Chin Health Serv Manage, 2022, 39(10): 736-741, 800. (in Chinese) [20] TAGHIZADEH S, FARHANGI M A, KHODAYARI-ZARNAQ R. Stakeholders perspectives of barriers and facilitators of childhood obesity prevention policies in Iran: a Delphi method study[J]. BMC Public Health, 2021, 21(1): 2260. doi: 10.1186/s12889-021-12282-7 [21] KUIJKEN N, VLOT-VAN ANROOIJ K, VAN SCHROJENSTEIN L V H, et al. Stakeholder expectations, roles and responsibilities in Dutch health promotion for people with intellectual disabilities[J]. Health Promot Int, 2019, 34(5): e59-e70. doi: 10.1093/heapro/day059 [22] 李薇薇. 价值冲突根源于利益冲突吗[J]. 道德与文明, 2012(3): 13-17. doi: 10.3969/j.issn.1007-1539.2012.03.002LI W W. Does value conflict stem from conflicts of interest?[J]. Moral Civilz, 2012(3): 13-17. (in Chinese) doi: 10.3969/j.issn.1007-1539.2012.03.002 [23] 卢丹凤, 韦朝毅. 论公共政策执行困境中的价值冲突[J]. 重庆工商大学学报(社会科学版), 2010, 27(1): 87-90. doi: 10.3969/j.issn.1672-0598.2010.01.014LU D F, WEI Z Y. Research on the value conflict in the difficulties of public policy implementation[J]. J Chongqing Technol Bus Univ(Soc Sci Edit), 2010, 27(1): 87-90. (in Chinese) doi: 10.3969/j.issn.1672-0598.2010.01.014 [24] 李永胜. 多元化背景下的价值冲突与价值整合[J]. 宁夏社会科学, 2006(4): 135-139. doi: 10.3969/j.issn.1002-0292.2006.04.033LI Y S. The value collision and value integration under the pluralism[J]. Ningxia Soc Sci, 2006(4): 135-139. (in Chinese) doi: 10.3969/j.issn.1002-0292.2006.04.033 [25] LANGE S J, MOORE L V, GALUSKA D A. Local government retail incentives for healthier food retailers in the USA, 2014[J]. Public Health Nutr, 2019, 22(13): 2521-2529. doi: 10.1017/S1368980019000983 [26] LINDHOLM R. Combating childhood obesity: a survey of laws affecting the built environments of low-income and minority children[J]. Rev Environ Health, 2011, 26(3): 155-167. doi: 10.1515/reveh.2011.023 [27] MICHAUD T L, ESTABROOKS P A, YOU W, et al. Effectiveness of incentives to improve the reach of health promotion programs: a systematic review and Meta-analysis[J]. Prev Med, 2022, 162: 107141. doi: 10.1016/j.ypmed.2022.107141 [28] FRIEDEN T R, DIETZ W, COLLINS J. Reducing childhood obesity through policy change: acting now to prevent obesity[J]. Health Aff (Millhood), 2010, 29(3): 357-363. doi: 10.1377/hlthaff.2010.0039 [29] CHRIQUI J F. Obesity prevention policies in U.S. States and localities: lessons from the field[J]. Curr Obes Rep, 2013, 2(3): 200-210. doi: 10.1007/s13679-013-0063-x [30] LAVERACK G. Public health: power, empowerment and professional practice[M]. New York: Palgrave Macmillan, 2005. [31] RAPPAPORT J, SEIDMAN E. Handbook of community psychology[M]. Boston: Springer, 2000: 43-63. [32] TEUFEL-SHONE N I, SIYUJA T, WATAHOMIGIE H J, et al. Community-based participatory research: conducting a formative assessment of factors that influence youth wellness in the Hualapai community[J]. Am J Public Health, 2006, 96(9): 1623-1628. doi: 10.2105/AJPH.2004.054254 -





 下载:
下载: