Acute effects of exposure to PM2.5 components on the lung function of primary school students
-
摘要:
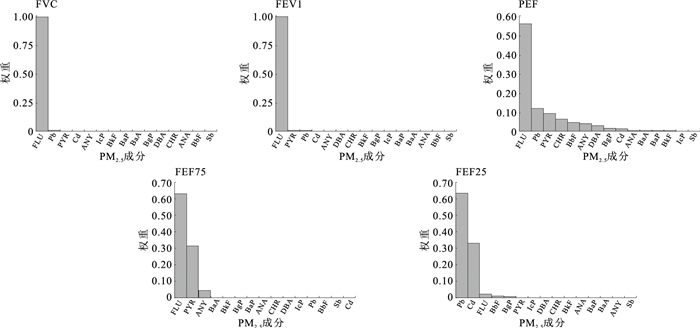
目的 分析细颗粒物(PM2.5)成分的混合暴露对小学生肺功能的急性影响,为保护儿童呼吸健康提供科学依据。 方法 2019—2021年,在天津市分层随机方法选取2 120名小学三至五年级学生进行肺功能测试。同时,结合PM2.5成分和学生住址,模拟短期暴露水平,并采用广义线性回归模型(GLM)和加权分数之和(WQS)回归模型分析PM2.5混合暴露对小学生肺功能的急性影响。 结果 2019—2021年天津市空气中PM2.5日均水平的平均值为81.14 μg/m3,高于国家标准。肺功能检测结果显示,天津市不同地区小学生的用力肺活量(FVC)、第1秒用力呼气量(FEV1)、最大呼气流量(PEF)、75%的用力呼气量(FEF75)和25%的用力呼气量(FEF25)等肺功能测量指标差异均无统计学意义(F值分别为1.23,0.87,2.34,1.56,0.98,P值均>0.05)。但GLM分析结果显示,空气中PM2.5各成分均对小学生的肺功能指标产生不利影响;当芴和芘的成分质量浓度每增加10 ng/m3时,小学生的肺功能FVC指标会分别降低166.44和61.94 L。WQS回归模型分析结果显示,在混合暴露对小学生肺功能指标的影响中,多环芳烃中的芴、芘以及重金属铅所占的比例权重较大。 结论 空气中PM2.5各成分的单一暴露和混合暴露均对小学生的肺功能指标产生不利影响,其中多环芳烃中的芴和芘以及重金属铅的影响尤为显著。应采取综合防治措施对可能的污染来源进行加强控制,以保护小学生的呼吸系统健康。 Abstract:Objective To analyze the acute effects of exposure to fine particulate matter (PM2.5) components on primary school students' lung function, so as to provide a scientific basis for protecting children's respiratory health. Methods From 2019 to 2021, the study selected a total of 2 120 primary school students from grades 3 to 5 in Tianjin using a stratified random sampling method to undergo lung function tests. At the same time, the short-term exposure levels were simulated by combining PM2.5 components and student addresses, and the acute impact of PM2.5 exposure on primary school students' lung function was analyzed by generalized linear models (GLM) and weighted quantile sum (WQS) regression models. Results The average daily concentration of PM2.5 in the air of Tianjin from 2019 to 2021 was 81.14 μg/m3, which was higher than the national standard. The results of lung function testing showed that there was no statistically significant difference in lung function measurement indicators such as forced vital capacity (FVC), forced expiratory volume at 1 second (FEV1), peak expiratory flow (PEF), 75% forced expiratory volume in 75 (FEF75), and 25% forced expiratory volume in 25 (FEF25) among primary school students in different regions of Tianjin (F=1.23, 0.87, 2.34, 1.56, 0.98, P>0.05). But the GLM analysis results showed that all components of PM2.5 in the air had adverse effects on the lung function indicators of primary school students. When the concentrations of fluorene (FLU) and pyrene (PYR) increased by 10 ng/m3, the FVC of primary school students decreased by 166.44 and 61.94 L respectively. The WQS regression model analysis results showed that the mixed exposure of PM2.5 components particularly significant damaging effects on lung function indicators in primary school students, especially the FLU and PYR components in polycyclic aromatic hydrocarbons, as well as the heavy metal lead. Conclusions Both single and mixed exposure to various PM2.5 components in the air have adverse effects on the lung function of primary school students. Among them, the influences of FLU and PYR in polycyclic aromatic hydrocarbons, as well as heavy metal Pb, are particularly significant.Potential pollution sources should be controlled to protect the respiratory health of primary school students by comprehensive prevention and control measures. -
Key words:
- Particulate matter /
- Environmental exposure /
- Lung /
- Regression analysis /
- Students
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 天津市2019—2021年不同地区儿童肺功能指标比较(x±s,L)
Table 1. Distribution of children's lung function indicators in Tianjin from 2019 to 2021(x±s, L)
地区 人数 FVC FEV1 PEF FEF75 FEF25 农村 1 212 2.47±0.92 2.37±0.96 4.40±2.49 2.79±1.25 4.27±2.47 城郊 606 1.58±0.40 1.49±0.37 2.68±0.67 1.83±0.64 2.27±0.93 城市 302 2.49±1.10 2.32±1.11 3.71±1.38 2.58±1.14 2.82±0.79 F值 1.23 0.87 2.34 1.56 0.98 P值 0.29 0.42 0.10 0.21 0.38 表 2 空气PM2.5各成分每增加10 ng/m3对小学生肺功能指标的影响[变化值(95%CI),L]
Table 2. Impact of increment of 10 ng/m3 in each component of ambient PM2.5 on the lung function indicators of primary school students[change value (95%CI), L]
成分 FVC FEV1 PEF FEF75 FEF25 Sb -1.44(-3.76~0.87) -1.29(-3.50~0.92) -2.03(-7.24~3.16) 2.05(-2.19~6.28) -8.16(-13.04~-3.32)a Cd -14.85(-30.04~0.25) -11.83(-26.33~2.60) -9.33(-43.94~24.87) 31.05(3.26~58.31) -54.54(-86.45~-22.57)a Pb -1.28(-1.73~-0.82)* -1.15(-1.58~-0.71)* -1.36(-2.41~-0.28)* -0.58(-1.46~0.31) -1.98(-2.97~-0.96)* FLU -166.44(-221.32~-112.31)* -179.32(-230.19~-129.01)* -477.50(-589.72~-366.11)* -161.21(-271.13~-55.33)* -371.53(-482.40~-256.46)* PYR -61.94(-89.73~-34.52)* -62.68(-88.93~-36.71)* -122.59(-182.46~-62.75)* -47.88(-99.47~2.62) -114.65(-171.07~-56.57)* ANY -10.71(-15.03~-6.45)* -11.53(-15.57~-7.53)* -28.50(-37.69~-19.37)* 1.72(-6.54~9.77) -31.79(-40.11~-23.23)* ANA -11.73(-17.14~-6.39)* -12.14(-17.24~-7.09)* -25.77(-37.63~-14.02)* 5.44(-4.68~15.31) -33.06(-43.68~-22.18)* CHR -12.06(-19.65~-4.58)* -11.95(-19.15~-4.83)* -21.23(-37.86~-4.70)* 7.92(-5.96~21.46) -27.45(-42.93~-11.49)* BaA -13.55(-21.81~-5.41)* -13.47(-21.30~-5.73)* -23.63(-41.46~-5.90)* 6.86(-8.08~21.43) -28.56(-45.12~-11.52)* BbF -6.87(-11.01~-2.78)* -6.76(-10.69~-2.87)* -12.64(-21.71~-3.63)* 6.83(-0.68~14.18) -19.41(-27.68~-10.89)* BkF -47.28(-74.64~-20.48)* -44.33(-70.27~-18.83)* -86.48(-146.07~-27.82)* 14.21(-36.55~62.99) -105.16(-159.33~-49.36)* BaP -18.67(-28.82~-8.66)* -18.38(-28.00~-8.87)* -38.65(-60.36~-17.01)* 8.49(-10.03~26.53) -46.39(-66.79~-25.17)* DBA -73.43(-112.32~-35.09)* -72.56(-109.43~-36.13)* -132.74(-217.87~-48.51)* -59.58(-131.69~10.71) -102.48(-182.03~-20.89)* BgP -19.55(-39.97~0.62) -18.12(-37.56~1.13) -44.06(-86.88~-1.04)* 32.27(-3.59~67.25) -28.02(-73.55~20.53) IcP -26.89(-40.36~-13.64)* -25.87(-38.64~-13.27)* -53.42(-82.54~-24.56)* 16.29(-8.59~40.32) -72.31(-98.78~-44.84)* 注: *P < 0.05。 -
[1] GARCIA E, RICE M B, GOLD D R. Air pollution and lung function in children[J]. J Allergy Clin Immunol, 2021, 148(1): 1-14. doi: 10.1016/j.jaci.2021.05.006 [2] THURSTON G D, KIPEN H, AANNESI-MAESANO I, et al. A joint ERS/ATS policy statement: what constitutes an adverse health effect of air pollution?An analytical framework[J]. Eur Respir J, 2017, 49(1): 1600419. doi: 10.1183/13993003.00419-2016 [3] SCHULTZ E S, LITONJUA A A, MELÉN E. Effects of long-term exposure to traffic-related air pollution on lung function in children[J]. Curr Allergy Asthma Rep, 2017, 17(6): 41. doi: 10.1007/s11882-017-0709-y [4] LUNDBERG B, GRUZIEVA O, ENEROTH K, et al. Air pollution exposure impairs lung function in infants[J]. Acta Paediatr, 2022, 111(9): 1788-1794. doi: 10.1111/apa.16412 [5] SCHULTZ E S, HALLBERG J, BELLANDER T, et al. Early-life exposure to traffic-related air pollution and lung function in adolescence[J]. Am J Respir Crit Care Med, 2016, 193(2): 171-177. doi: 10.1164/rccm.201505-0928OC [6] MILANZI E B, KOPPELMAN G H, SMIT H A, et al. Air pollution exposure and lung function until age 16 years: the PIAMA birth cohort study[J]. Eur Respir J, 2018, 52(3): 1800218. doi: 10.1183/13993003.00218-2018 [7] URMAN R, GARCIA E, BERHANE K, et al. The potential effects of policy-driven air pollution interventions on childhood lung development[J]. Am J Respir Crit Care Med, 2020, 201(4): 438-444. doi: 10.1164/rccm.201903-0670OC [8] MCGEACHIE M J, YATES K P, ZHOU X, et al. Patterns of growth and decline in lung function in persistent childhood asthma[J]. N Engl J Med, 2016, 374(19): 1842-1852. doi: 10.1056/NEJMoa1513737 [9] WANG G, HALLBERG J, FANER R, et al. Plasticity of individual lu-ng function states from childhood to adulthood[J]. Am J Respir Crit Care Med, 2023, 207(4): 406-415. doi: 10.1164/rccm.202203-0444OC [10] WANG X, DOCKERY D W, WYPIJ D, et al. Pulmonary function growth velocity in children 6 to 18 years of age[J]. Am Rev Respir Dis, 1993, 148(6 Pt 1): 1502-1508. [11] AGUSTÍ A, MELÉN E, DEMEO D L, et al. Pathogenesis of chronic obstructive pulmonary disease: understanding the contributions of gene-environment interactions across the lifespan[J]. Lancet Respir Med, 2022, 10(5): 512-524. doi: 10.1016/S2213-2600(21)00555-5 [12] ABDOLAHNEJAD A, JAFARI N, MOHAMMADI A, et al. Cardiovascular, respiratory, and total mortality ascribed to PM10 and PM2.5 exposure in Isfahan, Iran[J]. J Educ Health Promot, 2017, 6: 109. doi: 10.4103/jehp.jehp_166_16 [13] ZHANG L, MORISAKI H, WEI Y, et al. Characteristics of air pollutants inside and outside a primary school classroom in Beijing and respiratory health impact on children[J]. Environ Pollut, 2019, 255(Pt 1): 113147. [14] LIU P, ZHANG Y, WU T, et al. Acid-extractable heavy metals in PM(2.5) over Xi'an, China: seasonal distribution and meteorological influence[J]. Environ Sci Pollut Res Int, 2019, 26(33): 34357-34367. doi: 10.1007/s11356-019-06366-6 [15] BREIVIK K, ALCOCK R, LI Y F, et al. Primary sources of selected POPs: regional and global scale emission inventories[J]. Environ Pollut, 2004, 128(1/2): 3-16. [16] 李允, 高怡, 郑劲平. 《2021年ERS/ATS常规肺功能检查判读指南》的解读[J]. 中国循证医学杂志, 2022, 22(12): 1375-1381. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZXZ202212002.htmLI Y, GAO Y, ZHENG J P. Interpretation of the 2021 ERS/ATS Guidelines for the Interpretation of Routine Pulmonary Function Tests[J]. Chin J Evid Based Med, 2022, 22(12): 1375-1381. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZZXZ202212002.htm [17] 中华人民共和国环境保护部, 国家质量监督检验检疫总局. 环境空气质量标准: GB 3095—2012[S]. 北京: 中国环境科学出版社, 2012.Ministry of Ecology and Environment of the PRC, General Administration of Quality Supervision, Inspection and Quarantine of the PRC. Ambient air quality standards: GB 3095-2012[S]. Beijing: China Environmental Science Press, 2012. (in Chinese) [18] CAKMAK S, HEBBERN C, CAKMAK J D, et al. The influence of polycyclic aromatic hydrocarbons on lung function in a representative sample of the Canadian population[J]. Environ Pollut, 2017, 228: 1-7. doi: 10.1016/j.envpol.2017.05.013 [19] GARZA A, VEGA R, SOTO E. Cellular mechanisms of lead neurotoxicity[J]. Med Sci Monit, 2006, 12(3): Ra57-Ra65. [20] ARMSTRONG B G, GIBBS G. Exposure-response relationship between lung cancer and polycyclic aromatic hydrocarbons (PAHs)[J]. Occup Environ Med, 2009, 66(11): 740-746. doi: 10.1136/oem.2008.043711 [21] GAMMON M D, SANTELLA R M. PAH, genetic susceptibility and breast cancer risk: an update from the Long Island Breast Cancer Study Project[J]. Eur J Cancer, 2008, 44(5): 636-640. doi: 10.1016/j.ejca.2008.01.026 [22] HERTZ-PICCIOTTO I, BAKER R J, YAP P S, et al. Early childhood lower respiratory illness and air pollution[J]. Environ Health Perspect, 2007, 115(10): 1510-1518. doi: 10.1289/ehp.9617 [23] BRAGATO M, JOSHI K, CARLSON J B, et al. Combustion of coal, bagasse and blends thereof Part Ⅱ: speciation of PAH emissions[J]. 2011, 90(7): 51-58. -





 下载:
下载: