Analysis of potential categories of sexual behaviors among male students who have sex with men and the status of pre-exposure prophylaxis use
-
摘要:
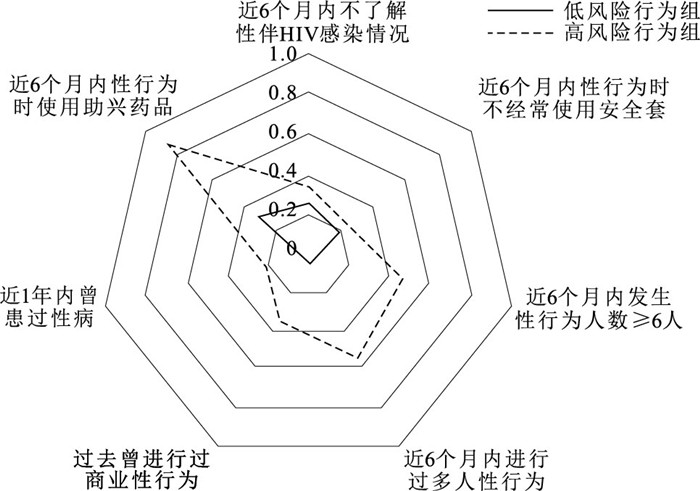
目的 使用潜在类别分析学生男男性行为者(MSM)中不同性行为模式人群暴露前预防(PrEP)使用情况,为确定符合MSM的PrEP使用模式提供依据。 方法 采用按比例抽样的方法对2021年10月20日至12月30日中国大陆31个省级行政区的MSM进行问卷调查,选择其中的1 040名学生纳入研究。对了解性伴HIV感染情况、使用安全套频率、性伴侣数量、进行过多人性行为、提供过商业性行为、使用助性药物以及近一年的性病史共7个性行为特征进行潜类别分析,并对人口学特征进行Logistic回归分析。调查不同性行为风险组的PrEP知晓率、使用意愿率和使用率。 结果 学生MSM可分为低风险性行为组(82.4%)和高风险性行为组(17.6%)2个潜在类别组。高风险性行为组的PrEP使用率(15.8%)更高,与低风险性行为组(7.2%)比较差异有统计学意义(χ2=13.43,P < 0.05)。居住在东北部、南部和西北部,居住地为试点城市和性角色为“0.5”(可能进行接受性和插入性性行为)的学生更可能属于高风险性行为组(OR值分别为3.13,3.07,3.87,2.22,1.66,P值均 < 0.05)。 结论 高风险与低风险性行为学生MSM作用PrEP的行为不同,应实施有针对性的干预措施,以促进PrEP在学生MSM中的使用,并降低该人群中感染HIV的风险。 Abstract:Objective To analyze the use of pre-exposure prophylaxis (PrEP) among male students who had sex with men (MSM) with different sexual behavior patterns using potential categories, so as to provide evidence for determining the use patterns of PrEP consistent with MSM. Methods A questionnaire survey was conducted by proportional sampling method on MSM in 31 provincial administrative regions in mainland China from 20 October to 30 December 2021, a total of 1 040 students were selected for the study. Latent variable analyses were conducted on a total of seven sexual behavioral characteristics, including knowledge of sexual partner HIV infection, frequency of condom use, number of sexual partners, engaging in group sex, provision of commercial sex, use of sex aids, and history of sexually transmitted infections (STIs) in the past year. And demographic characteristics were analyzed by Logistic regression analysis. The rates of PrEP awareness, willingness to use and usage rate in different sexual behavior risk groups were investigated. Results Student MSM could be divided into two potential category groups: a low-risk behavior group (82.4%) and a high-risk behavior group (17.6%). The PrEP usage rate (15.8%) was higher in the high-risk behavior group, and the difference was statistically significant compared to the low-risk behavior group (7.2%) (χ2=13.43, P < 0.05). Student MSM residing in the northeast, south, and northwest of China, in the pilot city, and with a sex role of "0.5" (possible acceptance and insertion of sexual behavior) were more likely to be in the high-risk behavior group (OR=3.13, 3.07, 3.87, 2.22, 1.66, P < 0.05). Conclusion Student MSM in high-risk and low-risk sexual differs in the behavior of PrEP, and targeted interventions should be implemented to promote the use of PrEP and reduce HIV infection in this population. -
Key words:
- Homosexuality, male /
- Pre-exposure prevention /
- Regression analysis /
- Students
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 各潜类别模型拟合指标比较
Table 1. Comparison of model fit metrics by latent class
类别数 Log-likelihood AIC值 BIC值 aBIC值 PLMRT值 PBLRT值 Entropy值 1 -3 211.01 6 436.02 6 470.65 6 448.41 — — — 2 -3 060.39 6 150.78 6 224.99 6 177.35 < 0.01 < 0.01 0.72 3 -3 042.66 6 131.32 6 245.10 6 172.05 0.08 < 0.01 0.71 4 -3 029.24 6 120.47 6 273.83 6 175.37 0.12 < 0.01 0.74 5 -3 018.40 6 114.80 6 307.73 6 183.86 0.16 — 0.65 表 2 不同性行为风险组学生MSM的社会人口学特征分布比较
Table 2. Comparison of socio-demographic distribution of MSM among students in different behavioural risk groups
组别 人数 文化程度 月收入 近6个月的肛交中角色 高中或中专 大专或本科 研究生及以上 无固定收入 <3 000元 ≥3 000元 1 0.5 0 低风险组 857 66(7.7) 647(75.5) 144(16.8) 618(72.1) 163(19.0) 76(8.9) 267(31.2) 165(19.3) 425(49.6) 高风险组 183 18(9.8) 136(74.3) 29(15.8) 119(65.0) 37(20.2) 27(14.8) 51(27.9) 52(28.4) 80(43.7) 合计 1 040 84(8.1) 783(75.3) 173(16.6) 737(70.9) 200(19.2) 103(9.9) 318(30.6) 217(20.9) 505(48.6) χ2值 0.96 6.46 7.67 P值 0.62 0.04 0.02 组别 人数 地理分区 是否为试点城市a 北部 东北部 东部 南部 西南部 西北部 中部 否 是 低风险组 857 149(17.4) 42(4.9) 273(31.8) 57(6.7) 107(12.5) 40(4.7) 189(22.0) 801(93.5) 56(6.5) 高风险组 183 32(17.5) 18(9.8) 52(28.4) 17(9.3) 14(7.7) 15(8.2) 35(19.1) 160(87.4) 23(12.6) 合计 1 040 181(17.4) 60(5.8) 325(31.3) 74(7.1) 121(11.6) 55(5.3) 224(21.5) 961(92.4) 79(7.6) χ2值 15.60 7.82 P值 0.02 0.01 注: a试点城市包括沈阳、北京、深圳和重庆;性角色为0.5指可能进行接受性和插入性性行为,0指进行接受性性行为,1指可能进行插入性性行为;()内数字为构成比/%。 -
[1] GBD 2017 HIV Collaborators. Global, regional, and national incidenc-e, prevalence, and mortality of HIV, 1980-2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the global burden of diseases, injuries, and risk factors study 2017[J]. Lancet HIV, 2019, 6(12): e831-e859. doi: 10.1016/S2352-3018(19)30196-1 [2] ROJAS P, MALOW R, RUFFIN B, et al. The HIV/AIDS epidemic in the dominican republic: key contributing factors[J]. J Int Assoc Phys AIDS Care (Chic), 2011, 10(5): 306-315. doi: 10.1177/1545109710397770 [3] HE N. Research progress in the epidemiology of HIV/AIDS in China[J]. China CDC Weekly, 2021, 3(48): 1022-1030. doi: 10.46234/ccdcw2021.249 [4] LAI J, PAN P, LIN Y, et al. A survey on HIV/AIDS-related knowledge, attitudes, risk behaviors, and characterivstics of men who have sex with men among university students in Guangxi, China[J]. Biomed Res Int, 2020, 2020: 7857231. [5] YANG Z, HUANG Z, DONG Z, et al. Prevalence of high-risky behaviors in transmission of HIV among high school and college student MSM in China: a Meta-analysis[J]. BMC Public Health, 2015, 15: 1272. doi: 10.1186/s12889-015-2614-4 [6] ANDERSON P L, GLIDDEN D V, LIU A, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men[J]. Sci Transl Med, 2012, 4(151): 151ra125. [7] SCHAEFER R, SCHMIDT H A, RAVASI G, et al. Adoption of guidelines on and use of oral pre-exposure prophylaxis: a global summary and forecasting study[J]. Lancet HIV, 2021, 8(8): e502-e510. doi: 10.1016/S2352-3018(21)00127-2 [8] MOLINA J M, CAPITANT C, SPIRE B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection[J]. N Engl J Med, 2015, 373(23): 2237-2246. doi: 10.1056/NEJMoa1506273 [9] LANZA S T, RHOADES B L. Latent class analysis: an alternative perspective on subgroup analysis in prevention and treatment[J]. Prev Sci, 2013, 14(2): 157-168. doi: 10.1007/s11121-011-0201-1 [10] WU Z, CHEN J, SCOTT S R, et al. History of the HIV epidemic in China[J]. Curr HIV/AIDS Rep, 2019, 16(6): 458-466. doi: 10.1007/s11904-019-00471-4 [11] 张北川, 刘明华, 于增照. 对男男性行为者艾滋病防治医学领域文献中某些内容和专用词的辨析[J]. 中国艾滋病性病, 2021, 27(9): 1021-1025. https://www.cnki.com.cn/Article/CJFDTOTAL-XBYA202109030.htmZHANG B C, LIU M H, YU Z Z. Identification of certain elements and terminology in the medical field of HIV prevention and treatment among men who have sex with men[J]. Chin J AIDS STD, 2021, 27(9): 1021-1025. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-XBYA202109030.htm [12] 郭佳欢, 康文婷, 刘童童, 等. 不同男男性行为者对PrEP使用意愿及影响因素分析[J]. 中国艾滋病性病, 2022, 28(12): 1375-1380. https://www.cnki.com.cn/Article/CJFDTOTAL-XBYA202212008.htmGUO J H, KANG W T, LIU T T, et al. Willingness of pre-exposure prophylaxis and influencing factors among different subgroups of men who have sex with men[J]. Chin J AIDS STD, 2022, 28(12): 1375-1380. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-XBYA202212008.htm [13] 曾宪华, 肖琳, 张岩波. 潜在类别分析原理及实例分析[J]. 中国卫生统计, 2013, 30(6): 815-817. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWT201306010.htmZENG X L, XIAO L, ZHANG Y B. Principle of latent class analysis and case analysis[J]. Chin J Health Stat, 2013, 30(6): 815-817. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWT201306010.htm [14] BARAKAT H, BARAKAT H, BAAJ M K. CVD and obesity in transitional syria: a perspective from the middle east[J]. Vasc Health Risk Manag, 2012, 8: 145-150. [15] FISHER D G, REYNOLDS G L, NAPPER L E. Use of crystal methamphetamine, viagra, and sexual behavior[J]. Curr Opin Infect Dis, 2010, 23(1): 53-56. doi: 10.1097/QCO.0b013e328334de0b [16] 何佳晋, 袁璐, 吴超. 2010—2019年中国艾滋病流行时空分布特征[J]. 中华疾病控制杂志, 2022, 26(5): 541-546. https://www.cnki.com.cn/Article/CJFDTOTAL-JBKZ202205009.htmHE J J, YUAN L, WU C. Temporal-spatial distribution of AIDS epidemic in China, 2010-2019[J]. Chin J Dis Control Prev, 2022, 26(5): 541-546. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-JBKZ202205009.htm [17] WANG H, ZHANG Y, MEI Z, et al. Protocol for a multicenter, real-world study of HIV pre-exposure prophylaxis among men who have sex with men in China (CROPrEP)[J]. BMC Infect Dis, 2019, 19(1): 721. doi: 10.1186/s12879-019-4355-y [18] CHEN H, YANG Y, HUANG Y, et al. Prevalence of poppers use and its sexual risks among men who have sex with men in southwestern China: a cross-sectional study[J]. BMC Public Health, 2018, 18(1): 1103. doi: 10.1186/s12889-018-6010-8 [19] TIEU H V, LI X, DONNELL D, et al. Anal sex role segregation and versatility among men who have sex with men: explore study[J]. J Acquir Immun Defic Syndr, 2013, 64(1): 121-125. doi: 10.1097/QAI.0b013e318299cede [20] OKAFOR C N, GORBACH P M, RAGSDALE A, et al. Correlates of preexposure prophylaxis (PrEP) use among men who have sex with men (MSM) in Los Angeles, California[J]. J Urban Health, 2017, 94(5): 710-715. doi: 10.1007/s11524-017-0172-z [21] SOUSA A F L, LIMA S, RIBEIRO C J N, et al. Adherence to pre-exposure prophylaxis (PrEP) among men who have sex with men (MSM) in Portuguese-Speaking Countries[J]. Int J Environ Res Public Health, 2023, 20(6): 4881. doi: 10.3390/ijerph20064881 [22] NEWCOMB M E, MORAN K, FEINSTEIN B A, et al. Pre-exposure prophylaxis (PrEP) use and condomless anal sex: evidence of risk compensation in a cohort of young men who have sex with men[J]. J Acquir Immun Defic Syndr, 2018, 77(4): 358-364. doi: 10.1097/QAI.0000000000001604 [23] CHAN P A, GLYNN T R, OLDENBURG C E, et al. Implementation of preexposure prophylaxis for human immunodeficiency virus prevention among men who have sex with men at a new england sexually transmitted diseases clinic[J]. Sex Transm Dis, 2016, 43(11): 717-723. -





 下载:
下载: