Differences in gut microbiota among primary school students with different levels of sugar-sweetened beverage consumption
-
摘要:
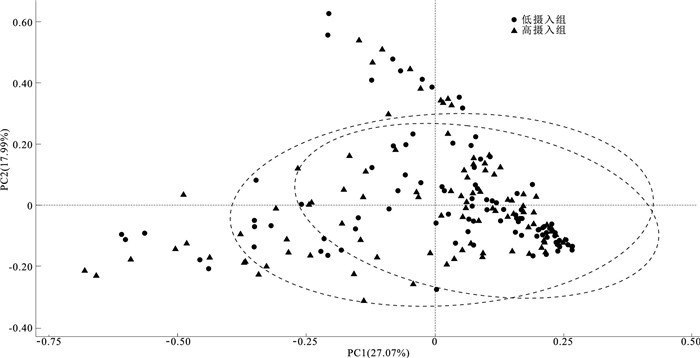
目的 探讨不同含糖饮料摄入水平小学生肠道菌群的差异,为更好地识别儿童健康风险并制定有针对性的健康政策提供科学依据。 方法 于2022年6月,采用分层整群随机抽样方法选取成都市健康小学生192名,采用膳食频率问卷调查含糖饮料摄入量,依据小学生每日含糖饮料摄入量中位水平分为低摄入组(96名)和高摄入组(96名)。使用16S rRNA高通量测序对两组小学生新鲜粪便标本进行肠道菌群检测,比较两组肠道菌群的多样性和群落结构差异。 结果 低摄入组小学生含糖饮料摄入量为(21.3±1.6) mL/d,高摄入组摄入量为(269.6±37.3)mL/d。多样性分析结果显示,低摄入组与高摄入组肠道菌群α多样性的可观测的OTU(Observed_otus)指数[298.50(259.75,342.25),305.50(244.25,367.75)],测序深度(Goods_coverage)指数[1.00(1.00,1.00),1.00(1.00,1.00)],Chao指数[304.18(260.75,348.78),305.88(245.68,370.88)],香农(Shannon)指数[5.88(5.29,6.45),5.71(4.89,6.28)],辛普森(Simpson)指数[0.95(0.91,0.97),0.94(0.88,0.97)]差异均无统计学意义(Z值分别为-0.64,-0.76,-0.54,-1.76,-1.67,P值均>0.05);两组肠道菌群的β多样性差异无统计学意义(R2=0.006,P>0.05)。在菌属水平,低摄入组中布劳特氏菌属[0.033(0.018,0.055)]、纺锤链杆属[0.009(0.005,0.015)]丰度均高于高摄入组[0.024(0.013,0.041),0.006(0.003,0.011)],差异均有统计学意义(Z值分别为-2.52,-2.81,P值均 < 0.05)。LEfSe分析显示两组菌群的组间差异主要体现在布劳特氏菌属、纺锤链杆属及八叠球菌属(LDA值分别为3.56,3.12,3.53,P值均 < 0.05)。 结论 不同含糖饮料摄入水平的小学生肠道菌群多样性和整体结构差异不大,但菌属水平存在物种差异,可为识别小学生的健康风险,制定健康对策提供科学依据。 Abstract:Objective To explore the differences in the gut microbiota of primary school students with different levels of sugar-sweetened beverage intake, so as to provide scientific evidence for better identification of health risks in children and the development of targeted health policies. Methods In June 2022, a total of 192 healthy primary school students from Chengdu were selected using a stratified cluster random sampling method. The sugar-sweetened beverage intake was assessed through a dietary frequency questionnaire. Based on the median daily sugar-sweetened beverage intake, primary school students were categorized into a low-intake group (n=96) and a high-intake group (n=96). The gut microbiota in fresh fecal samples from the two groups of primary school students was analyzed using 16S rRNA high-throughput sequencing, and the diversity and community structure differences in the gut microbiota were compared. Results Children in the low-intake group had a sugar-sweetened beverage intake of (21.3±1.6) mL/d, while the high-intake group had an intake of (269.6±37.3) mL/d. Diversity analysis results showed that there were no statistically significant differences between the low-intake and the high-intake group in terms of α diversity metrics: Observed_otus index [298.50 (259.75, 342.25), 305.50 (244.25, 367.75)], Goods_coverage index [1.00 (1.00, 1.00), 1.00 (1.00, 1.00)], Chao index [304.18 (260.75, 348.78), 305.88 (245.68, 370.88)], Shannon index [5.88 (5.29, 6.45), 5.71 (4.89, 6.28)] and Simpson index [0.95 (0.91, 0.97), 0.94 (0.88, 0.97)] (Z=-0.64, -0.76, -0.54, -1.76, -1.67, P>0.05). Furthermore, no statistically significant difference was observed in β diversity between the two groups (R2=0.006, P>0.05). At the genus level, the abundance of Blautia [0.033 (0.018, 0.055)] and Fusicatenibacter [0.009 (0.005, 0.015)] were higher in the low-intake group compared to the high-intake group [0.024 (0.013, 0.041), 0.006 (0.003, 0.011)]and differences were statistically significant (Z=-2.52, -2.81, P < 0.05). LEfSe analysis highlighted intergroup differences primarily in Blautia, Fusicatenibacter and Sarcina(LDA=3.56, 3.12, 3.53, P < 0.05). Conclusions There is no significant difference in the diversity and overall structure of the gut microbiota in primary school students with different levels of sugar-sweetened beverage intake. However, there are species variations at the genus level. The information can serve as a scientific basis for identifying health risks in primary school students and formulating targeted health strategies. -
Key words:
- Carbohydrates /
- Beverages /
- Feeding behavior /
- Gastrointestinal tract /
- Bacteria /
- Child
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 含糖饮料低摄入组与高摄入组小学生肠道菌群α多样性比较[M(P25, P75)]
Table 1. Comparison of α diversity in gut microbiota between low and high sugar-sweetened beverage intake groups among primary school students[M(P25, P75)]
组别 人数 可观测的OTU指数 测序深度指数 Chao指数 香农指数 辛普森指数 低摄入组 96 298.50(259.75, 342.25) 1.00(1.00, 1.00) 304.18(260.75, 348.78) 5.88(5.29, 6.45) 0.95(0.91, 0.97) 高摄入组 96 305.50(244.25, 367.75) 1.00(1.00, 1.00) 305.88(245.68, 370.88) 5.71(4.89, 6.25) 0.94(0.88, 0.97) Z值 -0.64 -0.76 -0.54 -1.76 -1.67 P值 0.53 0.45 0.59 0.08 0.10 表 2 含糖饮料低摄入组与高摄入组小学生肠道菌群在门水平相对丰度组间比较[M(P25, P75)]
Table 2. Comparison of relative abundances at the Phylum level in gut microbiota among primary school students between low and high sugar-sweetened beverage intake groups[M(P25, P75)]
组别 人数 厚壁菌门 拟杆菌门 变形菌门 放线菌门 低摄入组 96 0.59(0.46, 0.68) 0.27(0.15, 0.36) 0.03(0.01, 0.12) 0.02(0.01, 0.03) 高摄入组 96 0.56(0.37, 0.69) 0.25(0.13, 0.36) 0.06(0.01, 0.24) 0.02(0.01, 0.03) Z值 -0.82 -1.14 -1.60 -0.14 P值 0.40 0.30 0.10 0.90 表 3 含糖饮料低摄入组与高摄入组小学生肠道菌群在属水平相对丰度比较[M(P25, P75)]
Table 3. Comparison of relative abundances at the Genus level in gut microbiota among primary school students between low and high sugar-sweetened beverage intake groups[M(P25, P75)]
组别 人数 粪杆菌属 拟杆菌属 罗姆布茨菌属 普雷沃菌属 罗氏菌属 严格梭菌属 罕见小球菌属 假单胞菌属 双歧杆菌属 低摄入组 96 0.118(0.076, 0.188) 0.124(0.057, 0.237) 0.024(0.009, 0.074) 0.030(0.008, 0.083) 0.014(0.006, 0.023) 0.012(0.004, 0.027) 0.011(0.006, 0.016) 0.005(0.000, 0.080) 0.009(0.005, 0.022) 高摄入组 96 0.117(0.066, 0.177) 0.106(0.054, 0.202) 0.024(0.012, 0.078) 0.023(0.008, 0.129) 0.012(0.005, 0.022) 0.012(0.006, 0.028) 0.010(0.004, 0.014) 0.015(0.000, 0.191) 0.009(0.004, 0.027) Z值 -0.50 -1.03 -0.35 -0.55 -0.89 -0.30 -1.55 -1.35 -0.09 P值 0.60 0.30 0.70 0.60 0.40 0.80 0.10 0.20 0.90 组别 人数 琼脂杆菌属 另枝菌属 瘤胃球菌属 肠杆菌属 Ruminococcus_torques_group 副拟杆菌属 Eubacterium_coprostanoligenes_group 巨细胞菌属 小杆菌属 低摄入组 96 0.012(0.006, 0.023) 0.010(0.004, 0.021) 0.008(0.004, 0.017) 0.008(0.003, 0.014) 0.007(0.004, 0.014) 0.006(0.003, 0.013) 0.006(0.003, 0.016) 0.002(0.000, 0.006) 0.002(0.001, 0.005) 高摄入组 96 0.008(0.004, 0.019) 0.007(0.004, 0.016) 0.006(0.003, 0.015) 0.007(0.004, 0.015) 0.007(0.003, 0.012) 0.006(0.004, 0.010) 0.006(0.003, 0.011) 0.002(0.000, 0.006) 0.002(0.000, 0.005) Z值 -1.63 -1.13 -1.06 -0.25 -1.07 -0.46 -0.99 -0.18 -0.43 P值 0.10 0.30 0.30 0.80 0.30 0.60 0.30 0.90 0.70 表 4 含糖饮料低摄入组与高摄入组小学生肠道菌群的LEfSe相对丰度差异
Table 4. Differences of the relative abundance of LEfSe in gut microbiota among primary school students between low and high sugar-sweetened beverage intake groups
组别 微生物类群 LDA分值 低摄入组 布劳特氏菌属 3.56 纺锤链杆属 3.12 Clostridia_UCG_014 2.92 厌氧棒状菌属 2.91 挑剔真杆菌 2.75 凸腹真杆菌属 2.68 Erysipelotrichaceae_UCG_003 2.55 丁酸球菌属 2.41 肠球菌属 2.05 高摄入组 八叠球菌属 3.53 巨球型菌属 2.72 短波单胞菌属 2.39 鞘氨醇单胞菌属 2.37 皮肤杆菌属 2.34 TM7a 2.18 -
[1] 谢梦, 于冬梅, 赵丽云. 含糖饮料与儿童青少年超重肥胖关系[J]. 卫生研究, 2018, 47(5): 862-865, 870.XIE M, YU D M, ZHAO L Y. The relationship between sugary drinks and childhood adolescent overweight and obesity[J]. J Hyg Res, 2018, 47(5): 862-865, 870. (in Chinese) [2] 马冠生, 郑梦琪. 迫切需要控制儿童含糖饮料消费[J]. 中国学校卫生, 2017, 38(5): 641-643. doi: 10.16835/j.cnki.1000-9817.2017.05.001MA G S, ZHENG M Q. Urgent need to control children's consumption of sugary drinks[J]. Chin J Sch Health, 2017, 38(5): 641-643. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2017.05.001 [3] RAMPELLI S, GUENTHER K, TURRONI S, et al. Pre-obese children's dysbiotic gut microbiome and unhealthy diets may predict the development of obesity[J]. Commun Biol, 2018, 1: 222. doi: 10.1038/s42003-018-0221-5 [4] JASTROCH M, USSAR S, KEIPERT S. Gut microbes controlling blood sugar: no fire required![J]. Cell Metab, 2020, 31(3): 443-444. doi: 10.1016/j.cmet.2020.02.007 [5] TARASIUK A, FICHNA J. Gut microbiota: what is its place in pharmacology?[J]. Expert Rev Clin Pharmacol, 2019, 12(10): 921-930. doi: 10.1080/17512433.2019.1670058 [6] MOSZAK M, SZULIńSKA M, BOGDAńSKI P. You are what you eat—the relationship between diet, microbiota, and metabolic disorders: a review[J]. Nutrients, 2020, 12(4): 1096. doi: 10.3390/nu12041096 [7] RAMNE S, BRUNKWALL L, ERICSON U, et al. Gut microbiota composition in relation to intake of added sugar, sugar-sweetened beverages and artificially sweetened beverages in the malm offspring study[J]. Eur J Nutr, 2021, 60(4): 2087-2097. doi: 10.1007/s00394-020-02392-0 [8] BEARDS E, TUOHY K, GIBSON G. A human volunteer study to assess the impact of confectionery sweeteners on the gut microbiota composition[J]. Br J Nutr, 2010, 104(5): 701-708. doi: 10.1017/S0007114510001078 [9] ZHANG S, DANG Y. Roles of gut microbiota and metabolites in overweight and obesity of children[J]. Front Endocrinol (Lausanne), 2022, 13: 994930. doi: 10.3389/fendo.2022.994930 [10] DERRIEN M, ALVAREZ A S, DE VOS W M. The gut microbiota in the first decade of life[J]. Trends Microbiol, 2019, 27(12): 997-1010. doi: 10.1016/j.tim.2019.08.001 [11] 林琼希, 伦静娴, 张吉敏, 等. 学龄期儿童肉类食品摄入模式对其肠道菌群结构的影响[J]. 南方医科大学学报, 2021, 41(12): 1801-1808. doi: 10.12122/j.issn.1673-4254.2021.12.07LIN Q X, LUN J X, ZHANG J M, et al. Gut microbiome composition in pre-adolescentchildren with different meat consumption patterns[J]. J South Med Univ, 2021, 41(12): 1801-1808. (in Chinese) doi: 10.12122/j.issn.1673-4254.2021.12.07 [12] VALENTE H, TEIXEIRA V, PADRÃO P, et al. Sugar-sweetened beverage intake and overweight in children from a Mediterranean country[J]. Public Health Nutr, 2011, 14(1): 127-132. doi: 10.1017/S1368980010002533 [13] 史欣然, 安美静, 陈天娇, 等. 饮奶行为在家庭社会经济状况与儿童青少年体重指数间的中介作用[J]. 北京大学学报(医学版), 2021, 53(2): 308-313.SHI X R, AN M J, CHEN T J, et al. Mediating effect of milk intake between family socioeconomic status and body mass index of children and adolescents[J]. J Peking Univ(Health Sci), 2021, 53(2): 308-313. (in Chinese) [14] 李辉, 季成叶, 宗心南, 等. 中国0~18岁儿童、青少年体块指数的生长曲线[J]. 中华儿科杂志, 2009, 47(7): 493-498. doi: 10.3760/cma.j.issn.0578-1310.2009.07.004LI H, JI C Y, ZONG X N, et al. Body mass index growth curves for Chinese children and adolescents aged 0 to 18 years[J]. Chin J Pediatr, 2009, 47(7): 493-498. (in Chinese) doi: 10.3760/cma.j.issn.0578-1310.2009.07.004 [15] 段若男, 刘言, 薛红妹, 等. 成都市儿童青少年膳食质量评价及其与超重/肥胖的关系[J]. 中华流行病学杂志, 2014, 35(9): 994-997.DUAN R N, LIU Y, XUE H M, et al. Cross-sectional association between overall diet quality and overweight/obesity among children and adolescents in Chengdu[J]. Chin J Epidemiol, 2014, 35(9): 994-997. (in Chinese) [16] 杨月欣, 王光亚, 潘兴昌. 中国食物成分表[M]. 北京: 北京大学医学出版社, 2009.YANG Y X, WANG G Y, PAN X C. China food composition tables[M]. Beijing: Peking University Medical Press, 2009. (in Chinese) [17] 潘峰, 栾德春, 张彤薇, 等. 我国3岁及以上城市居民含糖饮料消费状况及其游离糖摄入评估[J]. 中国食品卫生杂志, 2022, 34(1): 126-130.PAN F, LUAN D C, ZHANG T W, et al. Assessment of sugar-sweetened beverages consumption and free sugar intake among urban residents aged 3 and above in China[J]. Chin J Food Hyg, 2022, 34(1): 126-130. (in Chinese) [18] GAN Q, XU P, YANG T, et al. Sugar-sweetened beverage consumption status and its association with childhood obesity among Chinese children aged 6-17 years[J]. Nutrients, 2021, 13(7): 2211. doi: 10.3390/nu13072211 [19] LEUNG C W, DIMATTEO S G, GOSLINER W A, et al. Sugar-sweetened beverage and water intake in relation to diet quality in U.S. children[J]. Am J Prev Med, 2018, 54(3): 394-402. doi: 10.1016/j.amepre.2017.11.005 [20] VAN LIPPEVELDE W, TE VELDE S J, VERLOIGNE M, et al. Associations between home- and family-related factors and fruit juice and soft drink intake among 10- to 12-year old children. The ENERGY project[J]. Appetite, 2013, 61(1): 59-65. [21] MORAN A J, SUBRAMANIAN S V, RIMM E B, et al. Characteristics associated with household purchases of sugar-sweetened beverages in US restaurants[J]. Obesity (Silver Spring), 2019, 27(2): 339-348. doi: 10.1002/oby.22380 [22] KEMP K M, ORIHUELA C A, MORROW C D, et al. Associations between dietary habits, sociodemographics, and gut microbial composition in adolescents[J]. Br J Nutr, 2024, 131(5): 809-820. doi: 10.1017/S0007114523002271 [23] SOPHA S C, MANEJWALA A, BOUTROS C N. Sarcina, a new threat in the bariatric era[J]. Hum Pathol, 2015, 46(9): 1405-1407. doi: 10.1016/j.humpath.2015.05.021 [24] 李蔚, 张强, 瞿嘉豪, 等. 大熊猫肠道菌群年龄演替规律分析[J]. 畜牧兽医学报, 2023, 54(6): 2619-2630.LI W, ZHANG Q, QU J H, et al. Analysis on the age succession of intestinal flora of giant panda[J]. Acta Vet Zootec Sin, 2023, 54(6): 2619-2630. (in Chinese) [25] RINNINELLA E, CINTONI M, RAOUL P, et al. Food components and dietary habits: keys for a healthy gut microbiota composition[J]. Nutrients, 2019, 11(10): 2393. doi: 10.3390/nu11102393 [26] GUTIÉRREZ-REPISO C, MORENO-INDIAS I, DE HOLLANDA A, et al. Gut microbiota specific signatures are related to the successful rate of bariatric surgery[J]. Am J Transl Res, 2019, 11(2): 942-952. [27] FENNEMA D, PHILLIPS I R, SHEPHARD E A. Trimethylamine and Trimethylamine N-Oxide, a Flavin-Containing Monooxygenase 3 (FMO3)-Mediated Host-Microbiome Metabolic Axis implicated in health and disease[J]. Drug Metab Dispos, 2016, 44(11): 1839-1850. doi: 10.1124/dmd.116.070615 [28] 蒋露芳, 王莹莹, 彭慧, 等. 学龄儿童肥胖与肠道菌群多样性及菌属丰度的关联研究[J]. 中华流行病学杂志, 2022, 43(2): 260-268. doi: 10.3760/cma.j.cn112338-20210617-00478JIANG L F, WANG Y Y, PENG H, et al. Association between obesity with the diversity and genus of gut microbiota in school-aged children[J]. Chin J Epidemiol, 2022, 43(2): 260-268. (in Chinese) doi: 10.3760/cma.j.cn112338-20210617-00478 [29] MACFARLANE G T, CUMMINGS J H. Probiotics and prebiotics: can regulating the activities of intestinal bacteria benefit health?[J]. West J Med, 1999, 171(3): 187-191. [30] LIU X, MAO B, GU J, et al. Blautia-a new functional genus with potential probiotic properties?[J]. Gut Microbes, 2021, 13(1): 1-21. [31] LIU C, LI J, ZHANG Y, et al. Influence of glucose fermentation on CO2 assimilation to acetate in homoacetogen Blautia coccoides GA-1[J]. J Ind Microbiol Biotechnol, 2015, 42(9): 1217-1224. doi: 10.1007/s10295-015-1646-1 [32] KIMURA I, INOUE D, MAEDA T, et al. Short-chain fatty acids and ketones directly regulate sympathetic nervous system via G protein-coupled receptor 41 (GPR41)[J]. Proc Natl Acad Sci USA, 2011, 108(19): 8030-8035. doi: 10.1073/pnas.1016088108 [33] KIMURA I, OZAWA K, INOUE D, et al. The gut microbiota suppresses insulin-mediated fat accumulation via the short-chain fatty acid receptor GPR43[J]. Nat Commun, 2013, 4: 1829. doi: 10.1038/ncomms2852 [34] OZATO N, SAITO S, YAMAGUCHI T, et al. Blautia genus associated with visceral fat accumulation in adults 20-76 years of age[J]. NPJ Biofilms Microb, 2019, 5(1): 28. doi: 10.1038/s41522-019-0101-x [35] JIN M, KALAINY S, BASKOTA N, et al. Faecal microbiota from patients with cirrhosis has a low capacity to ferment non-digestible carbohydrates into short-chain fatty acids[J]. Liver Int, 2019, 39(8): 1437-1447. doi: 10.1111/liv.14106 [36] GRYAZNOVA M, SMIRNOVA Y, BURAKOVA I, et al. Changes in the human gut microbiome caused by the short-term impact of lactic acid bacteria consumption in healthy people[J]. Probiotics Antimicrob Proteins, 2023. DOI: 10.1007/s12602-023-10111-4. [37] 杨启航, 蒲锐, 陈子扬, 等. 肠道菌群代谢物在肥胖调控中的作用与机制[J]. 中国组织工程研究, 2024, 28(2): 308-314. https://www.cnki.com.cn/Article/CJFDTOTAL-XDKF202402023.htmYANG Q H, PU R, CHEN Z Y, et al. Role and mechanism of intestinal flora metabolites in obesity regulation[J]. Chin J Tissue Engineer Res, 2024, 28(2): 308-314. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-XDKF202402023.htm [38] 沈丽萍, 汪正园, 史泽环, 等. 不同含糖饮料摄入频率儿童青少年体格发育和糖脂代谢指标的差异[J]. 环境与职业医学, 2023, 40(7): 761-768. https://www.cnki.com.cn/Article/CJFDTOTAL-LDYX202307005.htmSHEN L P, WANG Z Y, SHI Z H, et al. Associations of sugar-sweetened beverages intake frequency with physical growth and glucol-ipid metabolism among children and adolescents[J]. J Environ Occup Med, 2023, 40(7): 761-768. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-LDYX202307005.htm [39] 徐玉祥, 江伟康, 赵莉, 等. 含糖饮料摄入模式与儿童肥胖关联的纵向研究[J]. 中国学校卫生, 2021, 42(4): 506-509. doi: 10.16835/j.cnki.1000-9817.2021.04.007XU Y X, JIANG W K, ZHAO L, et al. A cohort study on the association between sugar-sweetened beverage intake and childhood obesity using a group-based trajectory model[J]. Chin J Sch Health, 2021, 42(4): 506-509. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2021.04.007 [40] 赵莉, 黎隐豪, 肖成汉, 等. 含糖饮料与儿童肥胖的关系及其防控政策研究进展[J]. 中国学校卫生, 2020, 41(3): 468-470. doi: 10.16835/j.cnki.1000-9817.2020.03.043ZHAO L, LI Y H, XIAO C H, et al. The relationship between sugary drinks and childhood obesity and advances in research and policies for prevention and control[J]. Chin J Sch Health, 2020, 41(3): 468-470. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2020.03.043 -





 下载:
下载: