Latent class analysis of sleep disturbances among children and adolescents with neurodevelopmental disorders in Tianjin
-
摘要:
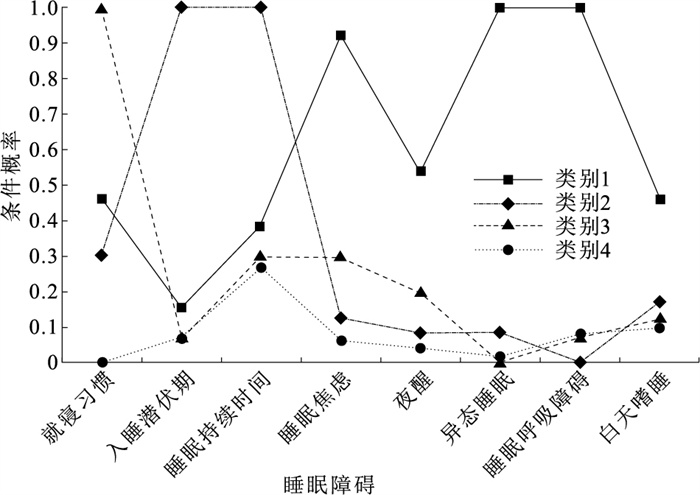
目的 了解天津市神经发育障碍儿童青少年睡眠障碍潜在类别及其与行为、社交问题的关系,为预防和改善神经发育障碍儿童青少年睡眠障碍提供依据。 方法 2021年9月至2024年6月,在天津市特殊教育学校和定点康复机构招募272名2~23岁神经发育障碍儿童青少年,采用儿童睡眠习惯问卷(CSHQ)评估睡眠障碍,孤独症儿童行为量表(ABC)、儿童孤独症评定量表(CARS)评估社交、行为问题及孤独症症状严重程度。采用潜在类别分析(LCA)将研究对象分为不同睡眠障碍类别,Cochran-Armitage检验分析不同年龄组睡眠障碍检出率的趋势性;采用Spearman秩相关分析各量表评分的关联,广义线性模型分析睡眠障碍对CARS、ABC量表得分的影响;采用协方差分析不同类别间儿童青少年行为、社交问题的差异。 结果 272名调查对象中,有197名(72.4%)神经发育障碍儿童青少年检出睡眠障碍。不同年龄组睡眠障碍检出率分别为2~6岁88.9%、7~12岁70.6%、13~18岁66.7%、19~23岁50.0%,随年龄增长呈下降趋势(Z=3.58,P < 0.01);CSHQ总分与ABC总分呈正相关(r=0.16,P=0.01)。广义线性模型分析表明,在调整年龄、性别、父母文化程度、家庭月总收入后,就寝习惯(β=3.60)和入睡潜伏期障碍(β=3.36)与CARS得分呈正相关,就寝习惯(β=16.73)和夜醒(β=17.46)与ABC得分呈正相关(P值均 < 0.05)。LCA分析表明,神经发育障碍儿童青少年睡眠障碍可分为4个类别;协方差分析结果显示,不同类别(类别1~4)研究对象CSHQ(70.84±9.05,50.96±6.64,50.33±5.82,43.84±5.44)和ABC(49.44±39.34,53.04±39.75,63.51±40.31,38.14±34.23)平均得分差异均有统计学意义(F值分别为92.09,3.95,P值均 < 0.05)。 结论 神经发育障碍儿童青少年睡眠障碍较严重且可分为不同潜在类别。 Abstract:Objective To understand the latent categories of sleep disturbances among children and adolescents with neurodevelopmental disorders (NDDs) in Tianjin and their relationship with behavioral and social issues, so as to provide a basis for preventing and improving sleep disturbances in the population. Methods From September 2021 to June 2024, 272 children and adolescents aged 2-23 years with neurodevelopmental disorders were recruited from special education schools and designated rehabilitation institutions in Tianjin. Sleep disturbances were assessed using the Children's Sleep Habits Questionnaire (CSHQ). Behavioral and social issues and severity were evaluated using the Autism Behavior Checklist (ABC) and Childhood Autism Rating Scale (CARS). Latent class analysis (LCA) was employed to categorize the subjects into different sleep disturbances categories. Cochran-Armitage test was used to analyze the trend of detection rate of sleep disturbances in different age groups. Spearman rank correlation was used to analyze the correlation between the scores of each scale. The generalized linear model was used to analyze the influence of CARS and ABC scale scores. Covariance analysis was used to examine differences in behavioral and social issues among the different categories. Results Among 272 survey respondents, a total of 197(72.4%) children and adolescents with NDDs were identified with sleep disturbances. The detection rates of sleep disturbances were 88.9% for those aged 2-6 years, 70.6% for aged 7-12, 66.7% for aged 13-18 and 50.0% for 19-23 years old, which was decreased across age group (Z=3.58, P < 0.01). There was a positive correlation between the total CSHQ score and the total ABC score (r=0.16, P=0.01). The generalized linear model analysis showed that after adjusting age, gender, parents' education level and family monthly income, bedtime habit (β=3.60) and sleeping latency disorder (β=3.36) were positively correlated with CARS scores, while the bedtime habit (β=16.73) and waking up at night (β=17.46) were positively correlated with ABC scores (P < 0.05). LCA revealed that sleep disturbances in children and adolescents with NDDs could be classified into four categories. The covariance analysis results showed that there were statistically significant differences in the average scores of CSHQ (70.84±9.05, 50.96±6.64, 50.33±5.82, 43.84±5.44) and ABC (49.44±39.34, 53.04±39.75, 63.51±40.31, 38.14±34.23) among different categories of all partipants (F=92.09, 3.95, P < 0.05). Conclusions Sleep disturbances in children and adolescents with NDDs are severe and exhibit distinct categorical characteristics. -
Key words:
- Neurodevelopmental disorders /
- Sleep /
- Latent class analysis /
- Child /
- Adolescent
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 不同性别和年龄神经发育障碍儿童青少年睡眠障碍检出率比较
Table 1. Comparison of sleep disturbances detection rates among children and adolescents with neurodevelopmental disorders by ages and genders
组别 选项 人数 统计值 睡眠障碍 就寝习惯 入睡潜伏期 睡眠持续时间 睡眠焦虑 夜醒 异态睡眠 睡眠呼吸障碍 白天嗜睡 性别 男 199 148(74.4) 42(21.1) 33(16.6) 69(34.7) 33(16.6) 19(9.6) 14(7.0) 23(11.6) 24(12.1) 女 73 49(67.1) 11(15.1) 9(12.3) 24(32.9) 6(8.2) 6(8.2) 4(5.5) 9(12.3) 10(13.7) χ2值 1.41 1.24 0.74 0.08 3.04 0.11 0.21 0.03 0.13 P值 0.24 0.27 0.39 0.78 0.08 0.74 0.65 0.86 0.72 年龄/岁 2~6 63 56(88.9) 21(33.3) 9(14.3) 27(42.9) 10(15.9) 6(9.5) 1(1.6) 3(4.8) 8(12.7) 7~12 119 84(70.6) 23(19.3) 17(14.3) 35(29.4) 19(16.0) 11(9.2) 13(10.9) 15(12.6) 14(11.8) 13~18 72 48(66.7) 6(8.3) 14(19.4) 27(37.5) 7(9.7) 5(6.9) 2(2.8) 10(13.9) 9(12.5) 19~23 18 9(50.0) 3(16.7) 2(11.1) 4(22.2) 3(16.7) 3(16.7) 2(11.1) 4(22.2) 3(16.7) Z值 3.58 3.18 -0.40 1.10 0.70 -0.21 -0.58 -2.13 -0.29 P值 < 0.01 < 0.01 0.69 0.27 0.49 0.83 0.57 0.03 0.77 合计 272 197(72.4) 53(19.5) 42(15.4) 93(34.2) 39(14.3) 25(9.2) 18(6.6) 32(11.8) 34(12.5) 注:()内数字为检出率/%。 表 2 不同年龄神经发育障碍儿童青少年睡眠时间比较(x±s)
Table 2. Comparison of sleep time among children and adolescents with neurodevelopmental disorders by ages(x±s)
年龄/岁 人数 平时晚上上床时间a 周末晚上上床时间a 平时晚上睡着时间a 周末晚上睡着时间a 平时早晨醒来时间a 周末早晨醒来时间a 平时早晨起床时间a 2~6 63 21:15±0.73 21:39±0.81 21:47±0.80 22:09±0.85 6:45±0.74 7:19±0.86 6:56±0.70 7~12 119 21:14±0.77 21:39±0.75 21:43±0.73 22:06±0.73 6:33±0.54 7:11±0.83 6:45±0.52 13~18 72 21:11±0.85 21:37±0.90 21:38±0.91 22:02±0.87 6:32±0.71 7:17±1.08 6:46±0.73 19~23 18 21:07±1.14 21:30±1.13 21:36±1.09 21:59±1.17 6:27±0.97 7:03±0.92 6:42±0.97 合计 272 21:13±0.81 21:38±0.83 21:42±0.82 22:05±0.83 6:35±0.68 7:23±1.72 6:48±0.66 F值 0.19 0.18 0.44 0.33 1.69 0.57 1.24 P值 0.90 0.91 0.73 0.81 0.17 0.64 0.30 年龄/岁 人数 周末早晨起床时间a 平时白天小睡时长/hb 周末白天小睡时长/hb 平时入睡用时/hb 周末入睡用时/hb 平时起床用时/hb 周末起床用时/hb 2~6 63 7:48±0.79 0.60(0.00, 0.90) 0.60(0.00, 1.20) 0.30(0.20, 0.40) 0.30(0.10, 0.50) 0.05(0.00, 0.20) 0.30(0.19, 0.30) 7~12 119 7:40±0.77 0.10(0.00, 0.60) 0.30(0.00, 0.60) 0.30(0.16, 0.30) 0.30(0.15, 0.30) 0.10(0.00, 0.20) 0.30(0.10, 0.30) 13~18 72 7:51±0.96 0.60(0.30, 0.90) 0.60(0.60, 0.90) 0.30(0.05, 0.30) 0.30(0.00, 0.30) 0.10(0.00, 0.20) 0.30(0.30, 0.30) 19~23 18 7:40±0.76 0.60(0.60, 0.71) 0.60(0.60, 1.20) 0.30(0.10, 0.60) 0.30(0.10, 0.60) 0.10(0.00, 0.30) 0.30(0.30, 0.06) 合计 272 7:54±1.68 0.60(0.00, 0.61) 0.60(0.00 0.90) 0.30(0.15, 0.30) 0.30(0.10, 0.30) 0.10(0.00, 0.20) 0.30(0.10, 0.30) F/H值 0.75 19.71 17.50 1.49 1.94 0.40 3.18 P值 0.52 < 0.01 < 0.01 0.69 0.58 0.94 0.37 注:a均数采用24 h制描述,标准差单位为小时数; b采用M(P25, P75)描述。 表 3 神经发育障碍儿童青少年睡眠障碍与行为、社交问题广义线性模型分析[β值(95%CI),n=272]
Table 3. Generalized linear model analysis of sleep disturbances and behavior and social disturbances of children and adolescents with neurodevelopmental disorders[β(95%CI), n=272]
自变量 CARS ABC 睡眠障碍 2.06(-0.81~4.92) 8.43(-1.99~18.85) 就寝习惯 3.60(0.35~6.86)* 16.73(4.92~28.54)* 入睡潜伏期 3.36(0.05~6.68)* 6.71(-6.37~19.79) 睡眠持续时间 0.15(-2.60~2.89) 3.73(-5.96~13.42) 睡眠焦虑 2.35(-1.58~6.28) 6.93(-7.06~20.92) 夜醒 4.30(-0.35~8.95) 17.46(2.17~32.74)* 异态睡眠 2.39(-3.01~7.78) 11.35(-8.52~31.22) 睡眠呼吸障碍 4.11(-0.00~8.21) 7.89(-7.94~23.73) 白天嗜睡 -1.32(-5.26~2.62) 5.22(-8.71~19.15) 注:各变量均以无为参照,*P < 0.05。 表 4 神经发育障碍儿童青少年睡眠障碍潜在类别分析(n=272)
Table 4. Potential class analysis of sleep disturbances in children and adolescents with neurodevelopmental disorders(n=272)
类别数 df AIC值 BIC值 aBIC值 Entropy PLMR值 PBLRT值 类别概率 1 8 1 792.91 1 821.76 1 796.39 — — — 1.00 2 17 1 693.99 1 755.29 1 701.39 0.995 < 0.01 < 0.01 0.95/0.05 3 26 1 687.57 1 781.32 1 698.88 0.850 0.56 0.02 0.84/0.11/0.05 4 35 1 681.32 1 807.52 1 696.55 0.966 < 0.01 0.03 0.72/0.15/0.08/0.05 5 44 1 682.39 1 841.05 1 701.53 0.959 0.06 0.04 0.72/0.14/0.09/0.03/0.03 表 5 不同潜在睡眠障碍类别神经发育障碍儿童青少年睡眠与行为、社交问题比较(x±s)
Table 5. Comparison of sleep with behavior and social problems in children and adolescents with neurodevelopmental disorders grouped by different potential sleep disturbances classes(x±s)
类别 人数 CSHQ CARS ABC 1 13 70.84±9.05 31.30±11.53 49.44±39.34 2 23 50.96±6.64 31.94±10.52 53.04±39.75 3 40 50.33±5.82 33.10±11.84 63.51±40.31 4 196 43.84±5.44 28.36±8.56 38.14±34.23 F值 92.09 2.54 3.95 P值 < 0.01 0.06 0.01 注:调整年龄、性别、父母文化程度、家庭月收入。 -
[1] 陈岑, 程慧, 江帆, 等. 孤独症谱系障碍儿童睡眠障碍的评估和干预[J]. 中国儿童保健杂志, 2022, 30(6): 637-641, 668.CHEN C, CHENG H, JIANG F, et al. Assessment and treatment for sleep disorders in children with autism spectrum disorder[J]. Chin J Child Health Care, 2022, 30(6): 637-641, 668. (in Chinese) [2] DAI X, WILLIAMS G J, GROEGER J A, et al. The role of circadian rhythms and sleep in the aetiology of autism spectrum disorder and attention-deficit/hyperactivity disorder: new evidence from bidirectional two-sample Mendelian randomization analysis[J]. Autism, 2025, 29(1): 76-86. doi: 10.1177/13623613241258546 [3] MARTINEZ-CAYUELAS E, MORENO-VINUéS B, PéREZ-SEBASTIáN I, et al. Sleep problems and circadian rhythm functioning in autistic children, autism with co-occurring attention deficit hyperactivity disorder, and typically developing children: a comparative study[J]. Autism, 2024, 28(12): 3167-3185. doi: 10.1177/13623613241254594 [4] TSE A C, YU C, LEE P H. Comparing sleep patterns between children with autism spectrum disorder and children with typical development: a matched case-control study[J]. Autism, 2020, 24(8): 2298-2303. doi: 10.1177/1362361320936827 [5] ASSOCIATION A P. Diagnostic and statistical manual of mental disorders[M]. 5th ed. Arlington, VA: American Psychiatric Association, 2013. [6] SADIKOVA E, DOVGAN K, MAZUREK M O. Longitudinal examination of sleep problems and symptom severity in children with autism spectrum disorder[J]. J Autism Dev Disord, 2023, 53(4): 1673-1681. doi: 10.1007/s10803-021-05401-1 [7] AATHIRA R, GULATI S, TRIPATHI M, et al. Prevalence of sleep abnormalities in Indian children with autism spectrum disorder: a cross-sectional study[J]. Pediatr Neurol, 2017, 74: 62-67. doi: 10.1016/j.pediatrneurol.2017.05.019 [8] DELIENS G, PEIGNEUX P. Sleep-behaviour relationship in children with autism spectrum disorder: methodological pitfalls and insights from cognition and sensory processing[J]. Dev Med Child Neurol, 2019, 61(12): 1368-1376. doi: 10.1111/dmcn.14235 [9] WELLER B E, BOWEN N K, FAUBERT S J. Latent class analysis: a guide to best practice[J]. J Black Psychol, 2020, 46(4): 287-311. doi: 10.1177/0095798420930932 [10] SCHREIBER J B. Latent class analysis: an example for reporting results[J]. Res Soc Adm Pharm, 2017, 13(6): 1196-1201. doi: 10.1016/j.sapharm.2016.11.011 [11] OWENS J A, SPIRITO A, MCGUINN M. The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children[J]. Sleep, 2000, 23(8): 1043-1051. http://www.depts.washington.edu/dbpeds/Screening%20Tools/CSHQ%20article.pdf [12] 李生慧, 金星明, 沈晓明, 等. 儿童睡眠习惯问卷中文版制定及测量性能考核[J]. 中华儿科杂志, 2007, 45(3): 176-180. doi: 10.3760/j.issn:0578-1310.2007.03.005LI S H, JIN X M, SHEN X M, et al. Development and psychometric properties of the Chinese version of Children's Sleep Habits Questionnaire[J]. Chin J Pediatr, 2007, 45(3): 176-180. (in Chinese) doi: 10.3760/j.issn:0578-1310.2007.03.005 [13] RELLINI E, TORTOLANI D, TRILLO S, et al. Childhood Autism Rating Scale (CARS) and Autism Behavior Checklist (ABC) correspondence and conflicts with DSM-IV criteria in diagnosis of autism[J]. J Autism Dev Disord, 2004, 34(6): 703-708. doi: 10.1007/s10803-004-5290-2 [14] SHUFFREY L C, RENNIE B, LI X, et al. Combining developmental and sleep health measures for autism spectrum disorder screening: an ECHO study[J]. Pediatr Res, 2024. DOI: 10.1038/s41390-024-03306-0. [15] CHAWLA J K, BERNARD A, HEUSSLER H, et al. Sleep, function, behaviour and cognition in a cohort of children with down syndrome[J]. Brain Sci, 2021, 11(10): 1317. doi: 10.3390/brainsci11101317 [16] MOHAMMED M A, ABDALKHALIG E M, ALI I A, et al. Pattern of sleep disorders among children with autism spectrum disorder[J]. BMC Psychiatry, 2024, 24(1): 539. doi: 10.1186/s12888-024-05981-z [17] LINDHOLM A, JARBIN H, AILI K, et al. Sex differences in children with uncomplicated attention deficit/hyperactivity disorder and sleep problems[J]. Children (Basel), 2024, 11(6): 616. [18] CUOMO B M, VAZ S, LEE E A L, et al. Effectiveness of sleep-based interventions for children with autism spectrum disorder: a Meta-synthesis[J]. Pharmacotherapy, 2017, 37(5): 555-578. doi: 10.1002/phar.1920 [19] SHUI A M, RICHDALE A L, KATZ T. Evaluating sleep quality using the CSHQ-autism[J]. Sleep Med, 2021, 87: 69-76. doi: 10.1016/j.sleep.2021.08.022 [20] 刘贝贝, 杜继鹏, 冯雪英, 等. 孤独症谱系障碍儿童的睡眠障碍及其相关因素分析[J]. 中国妇幼健康研究, 2021, 32(6): 838-846. doi: 10.3969/j.issn.1673-5293.2021.06.012LIU B B, DU J P, FENG X Y, et al. Sleeping problems and relevant factors in children with autism spectrum disorder[J]. Chin J Woman Child Health Res, 2021, 32(6): 838-846. (in Chinese) doi: 10.3969/j.issn.1673-5293.2021.06.012 [21] JOHNSON C R, BARTO L, WORLEY S, et al. Follow-up of telehealth parent training for sleep disturbances in young children with autism spectrum disorder[J]. Sleep Med, 2024, 119: 114-117. doi: 10.1016/j.sleep.2024.04.022 [22] CORTESE S, WANG F, ANGRIMAN M, et al. Sleep disorders in children and adolescents with autism spectrum disorder: diagnosis, epidemiology, and management[J]. CNS Drugs, 2020, 34(4): 415-423. doi: 10.1007/s40263-020-00710-y [23] SOMMERS L, PAPADOPOULOS N, FULLER-TYSZKIEWICZ M, et al. The connection between sleep problems and emotional and behavioural difficulties in autistic children: a network analysis[J]. J Autism Dev Disord, 2024. DOI: 10.1007/s10803-024-06298-2. [24] LI W, WANG G, YU Z, et al. Grandparental care and sleep disturbances in preschool children: a population-based prospective cohort study[J]. Sleep Med, 2021, 82: 165-171. doi: 10.1016/j.sleep.2021.03.033 [25] CHEN X Y, SHI X, ZHOU Y, et al. Change patterns of sleep problems predict mental health problems among adolescents: a 10-year cohort study of Chinese Wenchuan earthquake[J]. J Affect Disord, 2021, 287: 138-144. doi: 10.1016/j.jad.2021.02.080 [26] MCVEIGH J A, SMITH A, HOWIE E K, et al. Developmental trajectories of sleep during childhood and adolescence are related to health in young adulthood[J]. Acta Paediatr, 2021, 110(8): 2435-2444. doi: 10.1111/apa.15911 [27] HAN G T, TREVISAN D A, ABEL E A, et al. Associations between sleep problems and domains relevant to daytime functioning and clinical symptomatology in autism: a Meta-analysis[J]. Autism Res, 2022, 15(7): 1249-1260. doi: 10.1002/aur.2758 [28] VERHOEFF M E, BLANKEN L M E, KOCEVSKA D, et al. The bidirectional association between sleep problems and autism spectrum disorder: a population-based cohort study[J]. Mol Autism, 2018, 9: 8. doi: 10.1186/s13229-018-0194-8 -







 下载:
下载: