Association between alanine aminotransferase levels and cardiac structure in childhood
-
摘要:
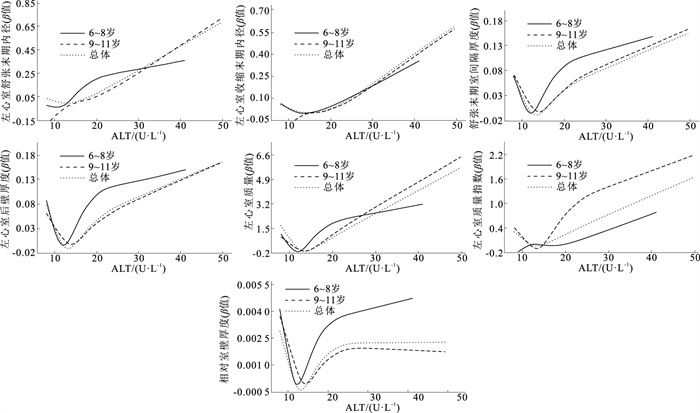
目的 探讨儿童期谷丙转氨酶(ALT)水平与心脏结构指标的关联,为促进儿童心脏健康提供科学依据。 方法 研究数据基于2017年11月—2018年1月开展的“桓台儿童心血管健康随访队列”基线调查,将数据完整的1 340名儿童纳入研究。采用问卷调查儿童的人口学信息和生活方式,并通过体格检查和血生化检测获取儿童的体质量指数(BMI)、血压、空腹血糖(FPG)、甘油三酯(TG)、高密度脂蛋白胆固醇(HDL-C)、低密度脂蛋白胆固醇(LDL-C)和谷丙转氨酶(ALT)等指标,通过超声检查测量儿童的左心室舒张末期内径(LVDD)、左心室收缩末期内径(LVSD)、左心室后壁厚度(LVPWT)以及舒张末期室间隔厚度(IVST),并计算相对室壁厚度(RWT)、左心室质量(LVM)和左心室质量指数(LVMI)。采用多元线性回归模型分析ALT水平对左心室结构指标的影响,采用限制性立方样条(RCS)模型探讨ALT水平与左心室结构指标的剂量-反应关系。 结果 不同ALT水平组儿童LVDD、LVSD、IVST、LVPWT、LVM、LVMI、RWT等心脏指标差异均有统计学意义(F值分别为78.69,60.08,72.86,74.89,83.14,36.70,20.46,P值均 < 0.05)。多元线性回归模型分析显示,调整可能协变量后,ALT水平与LVDD、LVSD、IVST、LVPWT、LVM、LVMI存在正相关(β值分别为0.10,0.20,0.16,0.16,0.23,0.18,P值均 < 0.05)。RCS模型分析显示,调整可能协变量后,儿童ALT水平与LVDD、LVSD、IVST和LVMI均存在线性剂量-反应关系(P非线性值均>0.05);ALT水平与LVPWT、LVM均存在非线性剂量反应关系(P非线性值均 < 0.05)。 结论 儿童期ALT水平与心脏多数结构指标呈正相关,且存在线性或非线性剂量-反应关系。 Abstract:Objective To explore the association between alanine aminotransferase (ALT) levels and cardiac structure in childhood, so as to provide scientific evidence to promote childhood cardiac health. Methods Data were obtained from the baseline survey of the "Huantai Childhood Cardiovascular Health Cohort Study" conducted from November 2017 to January 2018. A total of 1 340 children with complete data were included in the study. Demographic information and lifestyle factors were collected through questionnaires. Physical examinations and blood biochemical tests were performed to obtain children's body mass index (BMI), blood pressure, fasting plasma glucose (FPG), triglyceride (TG), high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), and ALT levels. Further, cardiac structural indicators such as left ventricular end-diastolic diameter (LVDD), left ventricular end-systolic diameter (LVSD), left ventricular posterior wall thickness (LVPWT), and interventricular septal thickness (IVST) were measured by ultrasound. Relative wall thickness (RWT), left ventricular mass (LVM), and left ventricular mass index (LVMI) were calculated. Multivariate linear regression models were used to analyze the relationship between ALT levels and cardiac structural indicators. Restricted cubic spline (RCS) models were used to explore the dose-response relationship between ALT levels and cardiac structural indicators. Results There were significant differences in LVDD, LVSD, IVST, LVPWT, LVM, LVMI and RWT in different ALT level groups (F=78.69, 60.08, 72.86, 74.89, 83.14, 36.70, 20.46, P < 0.05). Multivariate linear regression analysis showed that ALT levels were positively associated with LVDD, LVSD, IVST, LVPWT, LVM, and LVMI (β=0.10, 0.20, 0.16, 0.16, 0.23, 0.18, P < 0.05) after adjusting for potential covariates. The RCS showed a linear dose-response relationship between ALT levels and LVDD, LVSD, IVST, and LVMI after adjusting for potential covariates (Pnon-linear>0.05). In contrast, a non-linear dose-response relationship was found between ALT levels and LVPWT and LVM (Pnon-linear < 0.05). Conclusions ALT levels in childhood are positively associated with the majority of cardiac structural indicators, presenting a linear or non-linear dose-response relationship. -
Key words:
- Alanine aminotransferase /
- Heart /
- Regression analysis /
- Child
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 不同ALT水平组儿童人口学信息、生活方式、体格检查及血生化指标比较(x±s)
Table 1. Comparison of different demographic information, lifestyle, physical examination and blood biochemical parameters in children among different ALT levels of groups(x±s)
组别 人数 年龄/岁 身高/cm 体重/kg BMI/ (kg·m-2) 收缩压/ mmHg 舒张压/ mmHg 睡眠时间/ (h·d-1) ALT低水平组 424 8.04±1.55 133.06±10.53 29.88±7.76 16.63±2.39 104.09±8.96 62.35±6.36 9.34±0.47 ALT中水平组 410 8.46±1.51b 136.51±10.77b 33.69±9.04b 17.80±2.85b 106.03±8.30b 63.30±6.48 9.34±0.49 ALT高水平组 506 8.73±1.51bc 139.10±9.99bc 39.17±11.49bc 19.89±3.94bc 108.66±9.28bc 65.01±6.77bc 9.32±0.49 总体 1 340 8.43±1.55 136.40±10.70 34.55±10.44 18.22±3.47 106.41±9.08 63.65±6.64 9.33±0.48 F/H值 23.45 38.95 108.14 125.66 30.97 19.85 0.20 P值 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 0.82 组别 人数 视屏时间/ (h·d-1)a 体力活动时间/ (h·d-1)a FPG/ (mmol·L-1) TG/ (mmol·L-1)a HDL-C/ (mmol·L-1) LDL-C/ (mmol·L-1) ALT低水平组 424 0.64(0.64) 1.20(1.50) 4.66±0.57 0.62(0.30) 1.59±0.36 2.21±0.63 ALT中水平组 410 0.64(0.84) 1.20(1.30) 4.70±0.53 0.64(0.32) 1.61±0.38 2.22±0.69 ALT高水平组 506 0.64(0.81) 1.35(1.70) 4.82±0.56bc 0.74(0.47)bc 1.55±0.38c 2.37±0.70bc 总体 1 340 0.64(0.78) 1.20(1.50) 4.73±0.56 0.67(0.38) 1.58±0.38 2.27±0.68 F/H值 2.76 1.35 11.26 50.26 4.03 7.86 P值 0.25 0.51 < 0.01 < 0.01 0.02 < 0.01 注:a偏态分布,用中位数(四分位数间距)表示;1 mmHg=0.133 kPa;b与ALT低水平组相比,P < 0.05;c与ALT中水平组相比,P < 0.05。 表 2 不同ALT水平组儿童各心脏结构指标比较(x±s)
Table 2. Comparison of different cardiac structural indicators in children among different ALT levels of groups(x±s)
年龄/岁 ALT水平 人数 统计值 LVDD/mm LVSD/mm IVST/mm LVPWT/mm LVM/g LVMI/(g·m-2.7) RWT 6~8 低 262 37.50±1.07 23.90±1.37 5.47±0.26 5.62±0.26 52.30±5.09 27.75±3.23 0.30±0.01 中 187 38.02±1.49a 24.22±1.46a 5.58±0.36a 5.71±0.33a 54.92±7.47a 28.41±3.74 0.30±0.01 高 191 38.59±1.85ab 24.59±1.70ab 5.74±0.50ab 5.87±0.49ab 58.60±10.91ab 28.79±3.97b 0.30±0.02ab F值 30.99 11.88 27.65 27.01 35.09 4.83 8.10 P值 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 9~11 低 162 40.16±2.15 25.65±1.93 6.23±0.55 6.42±0.55 70.02±13.37 26.47±4.28 0.31±0.02 中 223 40.87±3.04 26.04±2.03 6.26±0.53 6.46±0.55 72.73±15.66 27.21±4.83 0.31±0.02 高 315 42.25±3.43ab 27.05±2.55ab 6.58±0.72ab 6.81±0.73ab 82.91±22.23ab 30.32±6.33ab 0.32±0.02b F值 28.76 24.87 25.14 27.72 33.42 34.93 4.28 P值 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 0.01 总体 低 424 38.51±2.04 24.56±1.82 5.76±0.54 5.92±0.56 59.07±12.58 27.26±3.71 0.30±0.02 中 410 39.57±2.84a 25.21±2.00a 5.95±0.57a 6.12±0.60a 64.61±15.41a 27.76±4.40 0.30±0.02 高 506 40.87±3.43ab 26.12±2.56ab 6.26±0.77ab 6.45±0.79ab 73.73±22.17ab 29.74±5.61ab 0.31±0.02ab F值 78.69 60.08 72.86 74.89 83.14 36.70 20.46 P值 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 < 0.01 注:a与ALT低水平组相比,P < 0.05;b与ALT中水平组相比,P < 0.05。 表 3 ALT水平与儿童心脏结构指标的多元线性回归分析(n=1 340)
Table 3. Multivariate linear regression analysis of ALT levels and cardiac structural indicators in children(n=1 340)
自变量 模型1 模型2 模型3 β值 标准误 P值 β值 标准误 P值 β值 标准误 P值 6~8岁 LVDD 0.20 0.03 < 0.01 0.20 0.03 < 0.01 0.06 0.03 0.04 LVSD 0.39 0.07 < 0.01 0.39 0.08 < 0.01 0.14 0.07 0.05 IVST 0.43 0.07 < 0.01 0.44 0.07 < 0.01 0.16 0.06 < 0.01 LVPWT 0.40 0.06 < 0.01 0.41 0.06 < 0.01 0.15 0.06 < 0.01 LVM 0.36 0.05 < 0.01 0.36 0.05 < 0.01 0.13 0.04 < 0.01 LVMI 0.22 0.06 < 0.01 0.22 0.06 < 0.01 0.13 0.06 0.04 RWT 0.15 0.04 < 0.01 0.15 0.04 < 0.01 0.07 0.04 0.09 9~11岁 LVDD 0.40 0.04 < 0.01 0.40 0.04 < 0.01 0.12 0.04 < 0.01 LVSD 0.65 0.07 < 0.01 0.65 0.07 < 0.01 0.22 0.06 < 0.01 IVST 0.59 0.07 < 0.01 0.59 0.07 < 0.01 0.16 0.06 < 0.01 LVPWT 0.62 0.07 < 0.01 0.62 0.07 < 0.01 0.17 0.06 < 0.01 LVM 0.78 0.07 < 0.01 0.78 0.07 < 0.01 0.26 0.06 < 0.01 LVMI 0.56 0.06 < 0.01 0.55 0.06 < 0.01 0.20 0.05 < 0.01 RWT 0.07 0.04 0.11 0.07 0.05 0.13 0.00 0.05 0.97 总体 LVDD 0.34 0.03 < 0.01 0.34 0.03 < 0.01 0.10 0.02 < 0.01 LVSD 0.57 0.05 < 0.01 0.57 0.05 < 0.01 0.20 0.05 < 0.01 IVST 0.55 0.05 < 0.01 0.55 0.05 < 0.01 0.16 0.04 < 0.01 LVPWT 0.56 0.05 < 0.01 0.56 0.05 < 0.01 0.16 0.04 < 0.01 LVM 0.65 0.05 < 0.01 0.66 0.05 < 0.01 0.23 0.04 < 0.01 LVMI 0.45 0.05 < 0.01 0.45 0.05 < 0.01 0.18 0.04 < 0.01 RWT 0.10 0.03 < 0.01 0.10 0.03 < 0.01 0.02 0.03 0.54 注:模型1,调整性别、年龄;模型2,在模型1基础上调整视屏时间、睡眠时间、体力活动时间、蔬菜水果摄入情况和碳酸饮料摄入情况;模型3,在模型2基础上调整BMI、收缩压、舒张压、FPG、TG、HDL-C、LDL-C;进行多元线性回归前对连续性变量进行归一化处理。 -
[1] 中国心血管健康与疾病报告编写组. 中国心血管健康与疾病报告2022概要[J]. 中国循环杂志, 2023, 38(6): 583-612. doi: 10.3969/j.issn.1000-3614.2023.06.001Writing Committee of the Report on Cardiovascular Health and Diseases in China. Report on cardiovascular health and diseases in China 2022: an updated summary[J]. Chin Circ J, 2023, 38(6): 583-612. (in Chinese) doi: 10.3969/j.issn.1000-3614.2023.06.001 [2] LEVY D, GARRISON R, SAVAGE D, et al. Prognostic implications of echocardiographically determined left ventricular mass in the framingham heart study[J]. N Engl J Med, 1990, 322(22): 1561-1566. doi: 10.1056/NEJM199005313222203 [3] DE JONG K A, CZECZOR J K, SITHARA S, et al. Obesity and type 2 diabetes have additive effects on left ventricular remodelling in normotensive patients: a cross sectional study[J]. Cardiovasc Diabetol, 2017, 16(1): 21-34. doi: 10.1186/s12933-017-0504-z [4] KAVEY R E. Left ventricular hypertrophy in hypertensive children and adolescents: predictors and prevalence[J]. Curr Hypertens Rep, 2013, 15(5): 453-457. doi: 10.1007/s11906-013-0370-3 [5] 席波. 重视儿童肥胖与近期亚临床心血管损害[J]. 中国学校卫生, 2019, 40(6): 803-804. doi: 10.16835/j.cnki.1000-9817.2019.06.002 XI B. Children obesity and short-term subclinical cardiovascular damage[J]. Chin J Sch Health, 2019, 40(6): 803-804. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2019.06.002 [6] 王欢. 儿童期腰围及其2年变化与颈动脉内中膜增厚和左心室肥厚的关联研究[D]. 济南: 山东大学, 2022.WANG H. Associations of waist circumference and its two-year changes with high carotid intima-media thickness and left ventricular hypertrophy in childhood[D]. Jinan: Shandong University, 2022. (in Chinese) [7] SOOKOIAN S, PIROLA C J. Liver enzymes, metabolomics and genome-wide association studies: from systems biology to the personalized medicine[J]. World J Gastroenterol, 2015, 21(3): 711-725. doi: 10.3748/wjg.v21.i3.711 [8] KWO P Y, COHEN S M, LIM J K. ACG clinical guideline: evaluation of abnormal liver chemistries[J]. Am J Gastroenterol, 2017, 112(1): 18-35. doi: 10.1038/ajg.2016.517 [9] ZHAO Y, YU Y, LI H, et al. The association between metabolic syndrome and biochemical markers in Beijing adolescents[J]. Int J Environ Res Public Health, 2019, 16(22): 4557-4567. doi: 10.3390/ijerph16224557 [10] WANG D D, LI Y, BHUPATHIRAJU S N, et al. Fruit and vegetable intake and mortality: results from 2 prospective cohort studies of US men and women and a Meta-analysis of 26 cohort studies[J]. Circulation, 2021, 143(17): 1642-1654. doi: 10.1161/CIRCULATIONAHA.120.048996 [11] YANG L, BOVET P, LIU Y, et al. Consumption of carbonated soft drinks among young adolescents aged 12 to 15 years in 53 low-and middle-income countries[J]. Am J Public Health, 2017, 107(7): 1095-1100. doi: 10.2105/AJPH.2017.303762 [12] DE SIMONE G, DANIELS S R, KIMBALL T R, et al. Evaluation of concentric left ventricular geometry in humans[J]. Hypertension, 2005, 45(1): 64-68. doi: 10.1161/01.HYP.0000150108.37527.57 [13] DEVEREUX R B, ALONSO D R, LUTAS E M, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings[J]. Am J Cardiol, 1986, 57(6): 450-458. doi: 10.1016/0002-9149(86)90771-X [14] DE SIMONE G, DANIELS S R, DEVEREUX R B, et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight[J]. J Am Coll Cardiol, 1992, 20(5): 1251-1260. doi: 10.1016/0735-1097(92)90385-Z [15] BELLENTANI S, BEDOGNI G, TIRIBELLI C. Liver and heart: a new link?[J]. J Hepatol, 2008, 49(2): 300-302. doi: 10.1016/j.jhep.2008.05.003 [16] LANG R M, BIERIG M, DEVEREUX R B, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology[J]. J Am Soc Echocardiogr, 2005, 18(12): 1440-1463. doi: 10.1016/j.echo.2005.10.005 [17] KELISHADI R, HEMATI Z, QORBANI M, et al. Association of alanine aminotransferase with different metabolic phenotypes of obesity in children and adolescents: the CASPIAN-V study[J]. Front Endocrinol (Lausanne), 2020, 11(8): 358-365. [18] PARK H K, HWANG J S, MOON J S, et al. Healthy range of serum alanine aminotransferase and its predictive power for cardiovascular risk in children and adolescents[J]. J Pediatr Gastroenterol Nutr, 2013, 56(6): 686-691. doi: 10.1097/MPG.0b013e31828b4e67 [19] MOHAMMADI F, QORBANI M, KELISHADI R, et al. Association of cardiometabolic risk factors and hepatic enzymes in a national sample of Iranian children and adolescents: the CASPIAN-Ⅲ study[J]. J Pediatr Gastroenterol Nutr, 2014, 58(4): 463-468. doi: 10.1097/MPG.0000000000000246 [20] KLEIN M, IAZZETTⅡ L, SPEISER P, et al. Alanine transferase: an independent indicator of adiposity related comorbidity risk in youth[J]. J Diabetes, 2015, 7(5): 649-656. doi: 10.1111/1753-0407.12221 [21] PATEL D A, SRINIVASAN S R, CHEN W, et al. Serum alanine aminotransferase and its association with metabolic syndrome in children: the Bogalusa heart study[J]. Metab Syndr Relat Disord, 2011, 9(3): 211-216. doi: 10.1089/met.2010.0086 [22] HEISKANEN J S, RUOHONEN S, ROVIO S P, et al. Determinants of left ventricular diastolic function: the cardiovascular risk in young finns study[J]. Echocardiography, 2019, 36(5): 854-861. doi: 10.1111/echo.14321 [23] YBARRA J, FERNANDEZ S, SANCHEZ-HERNANDEZ J, et al. Serum alanine aminotransferase predicts interventricular septum thickness and left ventricular mass in patients with nonalcoholic fatty liver disease[J]. Eur J Gastroenterol Hepatol, 2014, 26(6): 654-660. doi: 10.1097/MEG.0000000000000086 [24] LAZO M, RUBIN J, CLARK J M, et al. The association of liver enzymes with biomarkers of subclinical myocardial damage and structural heart disease[J]. J Hepatol, 2015, 62(4): 841-847. doi: 10.1016/j.jhep.2014.11.024 [25] SCHUSTEROVA I, LEENEN F H H, JURKO A, et al. Epicardial adipose tissue and cardiometabolic risk factors in overweight and obese children and adolescents[J]. Pediatr Obes, 2014, 9(1): 63-70. doi: 10.1111/j.2047-6310.2012.00134.x [26] VERGANI L. Fatty acids and effects on in vitro and in vivo models of liver steatosis[J]. Curr Med Chem, 2019, 26(19): 3439-3456. doi: 10.2174/0929867324666170518101334 [27] BADIMON L, PENA E, ARDERIU G, et al. C-reactive protein in atherothrombosis and angiogenesis[J]. Front Immunol, 2018, 9(3): 430-437. [28] SU L, ZHANG J, GOMEZ H, et al. Reactive oxygen species-induced lipid peroxidation in apoptosis, autophagy, and ferroptosis[J]. Oxid Med Cell Longev, 2019, 2019: 5080843. [29] KUNUTSOR S K, APEKEY T A, KHAN H. Liver enzymes and risk of cardiovascular disease in the general population: a Meta-analysis of prospective cohort studies[J]. Atherosclerosis, 2014, 236(1): 7-17. doi: 10.1016/j.atherosclerosis.2014.06.006 [30] KOUTNY F, WEGHUBER D, BOLLOW E, et al. Prevalence of prediabetes and type 2 diabetes in children with obesity and increased transaminases in European German-speaking countries. Analysis of the APV initiative[J]. Pediatr Obes, 2020, 15(4): e12601. doi: 10.1111/ijpo.12601 [31] AROOR A R, MCKARNS S, DEMARCO V G, et al. Maladaptive immune and inflammatory pathways lead to cardiovascular insulin resistance[J]. Metabolism, 2013, 62(11): 1543-1552. doi: 10.1016/j.metabol.2013.07.001 [32] WANG M, LI Y, LI S, et al. Endothelial dysfunction and diabetic cardiomyopathy[J]. Front Endocrinol (Lausanne), 2022, 13(4): 851941. -







 下载:
下载: