Analysis of the effect of 12-week high-intensity fitness exercises on improving metabolic disorders among obese adolescents
-
摘要:
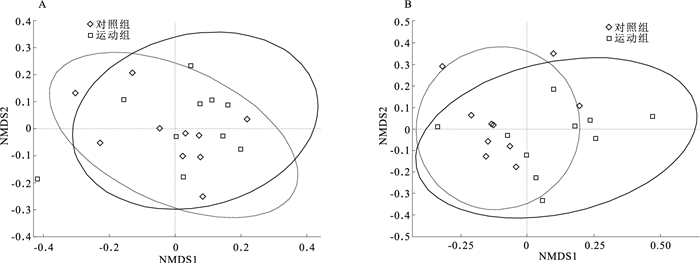
目的 分析12周中高强度健身操对肥胖青少年身体成分、脂代谢及肠道菌群的影响,为改善肥胖青少年健康水平提供参考。 方法 于2023年1—6月,招募淮安市华丰职业技术学校20名肥胖青少年纳入研究,采用随机数字表法将受试者分配到运动组(10名)和对照组(10名),进行为期12周运动干预,两组干预期间进食相同。运动组每周进行3次运动,以中高强度的有氧运动配合高强度间歇为主,第1周30 min有氧运动,以后每周在总干预时间中有10 min高强度间歇训练,其余时间皆进行有氧运动,总干预时间达到60 min保持;对照组不接受特定干预。采用生物电阻抗原理测量身体成分及全自动分析生化仪检测血脂水平,在基线和干预12周后测定血清炎症因子表达水平,并用16S rRNA基因测序技术测定肠道菌群。采用χ2检验、t检验进行统计学分析。 结果 干预12周后,运动组肥胖青少年甘油三酯(TG)和低密度脂蛋白胆固醇(LDL-C)水平分别由(1.7±0.6,3.5±0.8)mmol/L下降至(0.9±0.3,2.6±0.4)mmol/L,高密度脂蛋白胆固醇(HDL-C)由(1.1±0.2)mmol/L提升至(1.4±0.2)mmol/L;运动组血清白细胞介素-1受体拮抗剂(IL-1Rn)由(8.4±1.6)ng/mL降至(4.5±0.4)ng/mL(t值分别为7.34, 2.49,-3.05, 2.56,P值均 < 0.05)。α多样性结果显示,运动组Chao指数(268.00±22.67)、Ace指数(243.98±38.64)均高于对照组(184.52±19.28, 171.43±23.33),差异均有统计学意义(t值分别为2.48, 2.53, P值均 < 0.05);运动组Shannon指数(5.36±1.41)高于对照组(4.73±1.12),Simpson指数(0.78±0.10)低于对照组(0.89±0.10),但差异均无统计学意义(t值分别为1.83, -2.10, P值均>0.05)。β多样性结果显示,运动组与对照组肠道菌群结构的组间差异大于组内差异,运动组与对照组的肠道菌群结构差异有统计学意义(R2=0.083,P < 0.05);干预后,运动组与对照组肥胖青少年肠道菌群在属、纲、种和科水平上相对丰度差异均有统计学意义(P值均 < 0.05)。 结论 12周中高强度健身操能够通过肠道菌群-脂代谢途径减轻单纯性肥胖青少年患者肥胖症状,改善低度慢性炎症状态。 Abstract:Objective To analyze the effects of 12-week high-intensity fitness exercise on body composition, lipid metabolism and gut microbiota in obese adolescents, so as to provide references for improving the health levels of obese adolescents. Methods From January to June 2023, 20 obese adolescents from Huaifeng Vocational and Technical School in Huai'an City were recruited for the study. Participants were assigned to an exercise group (n=10) and a control group (n=10) for a 12-week exercise intervention by random number table method, and both groups had the same diet during the intervention period. The exercise group engaged in three exercises every week, mainly consisting of moderate to high-intensity aerobic exercise combined with high-intensity intervals. In the first week, there was a 30 minutes of aerobic exercise, followed by 10 minutes of high-intensity interval training in the total intervention time each week, and the rest of the time was aerobic exercise with a total intervention time of 60 minutes to maintain; the control group did not receive specific interventions. Body composition was measured using bioelectrical impedance analysis, and lipid levels were determined using an automatic biochemical analyzer. The expression levels of serum inflammatory factors were measured at baseline and after 12 weeks of intervention, and gut microbiota was analyzed using 16S rRNA gene sequencing. Statistical analysis was performed using t test and Chi-square test. Results After 12 weeks of intervention, the levels of triglycerides (TG), and low-density lipoprotein cholesterol (LDL-C) in obese adolescents in the exercise group decreased from (1.7±0.6, 3.5±0.8) mmol/L to (0.9±0.3, 2.6±0.4) mmol/L, while high-density lipoprotein cholesterol (HDL-C) increased from (1.1±0.2) mmol/L to (1.4±0.2) mmol/L; and serum interleukin-1 receptor antagonist(IL-1Rn) decreased from (8.4±1.6) to (4.5±0.4) ng/mL in the exercise group (t=7.34, 2.49, -3.05, 2.56, P < 0.05). The α-diversity results showed that the Chao index (268.00±22.67) and Ace index (243.98±38.64) in the exercise group were higher than those in the control group (184.52±19.28, 171.43±23.33), and the differences were statistically significant (t=2.48, 2.53, P < 0.05). The Shannon index (5.36±1.41) in the exercise group was higher than that in the control group (4.73±1.12), and the Simpson index (0.78±0.10) was lower than that in the control group (0.89±0.10), but the differences were not statistically significant (t=1.83, -2.10, P>0.05). The β-diversity results showed that the intergroup differences in gut microbiota structure between the exercise group and the control group were greater than the intragroup differences, and the differences in gut microbiota structure between the exercise group and the control group were statistically significant (R2=0.083, P < 0.05). After intervention, there were significant differences in the relative abundances at the levels of phylum, class, genus, and species in gut microbiota among obese adolescents between the exercise group and the control group (P < 0.05). Conclusion The 12-week high-intensity fitness exercise can alleviate obesity symptoms in obese adolescents through the gut microbiota-lipid metabolism pathway and improve mild chronic inflammatory status. -
Key words:
- Physical education and training /
- Obesity /
- Metabolism /
- Intervention students /
- Adolescent
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 两组肥胖青少年干预前后各指标比较(x±s)
Table 1. Comparison of indicators before and after intervention among obese adolescents in two groups(x±s)
组别 干预前后 统计值 体重/kg BMI/(kg·m-2) 腰围/cm 臀围/cm 体脂率/% FPG/(mmol·L-1) 运动组 干预前 94.8±8.0 33.0±4.1 103.7±6.6 111.1±6.7 33.9±4.4 5.6±0.8 (n=10) 干预后 89.8±13.4 26.3±4.0 84.0±10.4 94.1±8.8 28.9±5.5 5.2±0.4 t值 1.55 2.74 7.97 2.52 6.25 5.94 P值 0.13 0.03 < 0.01 0.04 < 0.01 < 0.01 对照组 干预前 93.3±15.2 31.9±2.6 99.3±10.2 110.4±6.3 35.1±4.1 5.6±0.4 (n=10) 干预后 94.1±13.2 31.1±3.2 100.1±8.3 108.2±6.7 35.1±5.4 5.6±0.6 t值 -1.51 0.45 -1.69 2.01 0.79 1.01 P值 0.13 0.55 0.13 0.06 0.49 0.38 组别 干预前后 统计值 TC/(mmol·L-1) TG/(mmol·L-1) HDL-C/(mmol·L-1) LDL-C/(mmol·L-1) IL-1β/(ng·mL-1) IL-1Rn/(ng·mL-1) 运动组 干预前 5.0±0.8 1.7±0.6 1.1±0.2 3.5±0.8 1.9±0.2 8.4±1.6 (n=10) 干预后 4.1±0.4 0.9±0.3 1.4±0.2 2.6±0.4 0.7±0.4 4.5±0.4 t值 2.01 7.34 -3.05 2.49 0.42 2.56 P值 0.07 < 0.01 0.02 0.04 0.69 0.02 对照组 干预前 5.1±0.6 1.5±0.4 1.3±0.2 3.5±0.6 1.9±0.1 8.4±1.3 (n=10) 干预后 4.9±0.9 1.5±0.3 1.3±0.3 3.4±0.7 1.9±0.3 8.3±1.4 t值 7.65 1.09 1.99 1.53 1.74 0.37 P值 < 0.01 0.32 0.07 0.16 0.11 0.78 表 2 两组肥胖青少年干预后不同分类水平物种相对丰度比较(x±s)
Table 2. Comparison of indicators before and after intervention for obese adolescents in two groups(x±s)
组别 人数 属水平 纲水平 另枝菌属 琥珀酸弧菌科
(UCG-002)毛螺菌科(NK4A136) 革兰阳性菌 梭状芽孢杆菌 运动组 10 37.30±3.21 19.93±1.69 2.98±0.73 1.73±0.18 32.38±11.41 对照组 10 6.08±1.30 2.01±0.41 1.19±0.13 6.92±0.46 23.02±7.56 t值 2.60 2.58 2.13 3.07 2.37 P值 0.02 0.02 0.04 0.01 0.05 组别 人数 种水平 科水平 腐烂别样杆菌 毛螺旋菌
(GAM79)肥胖别样杆菌 沙别样杆菌 文肯菌科 颤螺旋菌科 运动组 10 27.76±2.63 2.98±0.37 1.45±0.18 27.78±2.88 37.39±3.22 29.81±2.77 对照组 10 6.91±1.11 1.19±0.13 15.93±3.58 6.81±1.06 6.08±1.34 3.79±0.54 t值 2.89 2.21 2.28 2.29 2.54 2.43 P值 0.01 0.04 0.05 0.05 0.02 0.02 -
[1] VACCA M, CELANO G, CALABRESE F M, et al. The controversial role of human gut lachnospiraceae[J]. Microorganisms, 2020, 8(4): 573. doi: 10.3390/microorganisms8040573 [2] BAQUERO F, NOMBELA C. The microbiome as a human organ[J]. Clin Microbiol Infect, 2012, 18(Suppl 4): 2-4. http://www.zhangqiaokeyan.com/journal-foreign-detail/070401799387.html [3] MA L, NI Y, WANG Z, et al. Spermidine improves gut barrier integrity and gut microbiota function in diet-induced obese mice[J]. Gut Microbes, 2020, 12(1): 1-19. [4] MILLION M, LAGIER J C, YAHAV D, et al. Gut bacterial microbiota and obesity[J]. Clin Microbiol Infect, 2013, 19(4): 305-313. doi: 10.1111/1469-0691.12172 [5] YATSUNENKO T, REY F E, MANARY M J, et al. Human gut microbiome viewed across age and geography[J]. Nature, 2012, 486(7402): 222-227. doi: 10.1038/nature11053 [6] HOLLISTER E B, RIEHLE K, LUNA R A, et al. Structure and function of the healthy pre-adolescent pediatric gut microbiome[J]. Microbiome, 2015, 3: 36. doi: 10.1186/s40168-015-0101-x [7] LOVE-GREGORY L, ABUMRAD N A. CD36 genetics and the metabolic complications of obesity[J]. Curr Opin Clin Nutr Metab Care, 2011, 14(6): 527-534. doi: 10.1097/MCO.0b013e32834bbac9 [8] 袁久术, 周明阳, 冷玉琳, 等. 基于肠道菌群失调探讨"升清降浊"理论在糖尿病周围神经病变中的作用[J]. 世界科学技术-中医药现代化, 2023, 25(4): 1494-1501. https://www.cnki.com.cn/Article/CJFDTOTAL-SJKX202304035.htmYUAN J S, ZHOU M Y, LENG Y L, et al. Exploring the role of the theory of ascending lucidity and descending turbidity in diabeticperipheral neuropathy based on intestinal microbiota lmbalance[J]. Mod Trad Chin Med Mater Med World Sci Technol, 2023, 25(4): 1494-1501. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-SJKX202304035.htm [9] SUN Y, WU D, ZENG W, et al. The role of intestinal dysbacteriosis induced arachidonic acid metabolism disorder in inflammaging in atherosclerosis[J]. Front Cell Infect Microbiol, 2021, 11: 618265. doi: 10.3389/fcimb.2021.618265 [10] JU M, LIU Y, LI M, et al. Baicalin improves intestinal microecology and abnormal metabolism induced by high-fat diet[J]. Eur J Pharm, 2019, 857: 172457. doi: 10.1016/j.ejphar.2019.172457 [11] 冷思逸, 蒲锐, 刘辉. 运动调控肠道菌群防治神经退行性疾病的研究进展[J]. 生命科学, 2023, 35(11): 1498-1507. https://www.cnki.com.cn/Article/CJFDTOTAL-SMKX202311010.htmLENG S Y, PU R, LIU H. Research progress of exercise regulating qut microbiota to modulate neurodegenerative disease[J]. Chin Bull Life Sci, 2023, 35(11): 1498-1507. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-SMKX202311010.htm [12] 岑凤. 植物甾醇豆甾醇联合有氧运动对肥胖大鼠肠道菌群和肝脏脂代谢的影响[J]. 分子植物育种, 2023, 21(19): 6523-6530. https://www.cnki.com.cn/Article/CJFDTOTAL-FZZW202319034.htmCEN F. Impact of plant sterol combined with aerobic exercise on gut microbiota and hepatic lipidmetabolism in obese rats[J]. Mol Plant Breed, 2023, 21(19): 6523-6530. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-FZZW202319034.htm [13] 杨启航, 蒲锐, 陈子扬, 等. 肠道菌群与骨质疏松及运动干预[J]. 中国组织工程研究, 2024, 28(26): 4250-4256. https://www.cnki.com.cn/Article/CJFDTOTAL-XDKF202426023.htmYANG Q H, PU R, CHEN Z Y, et al. Intestinal flora and osteoporosis and exercise intervention[J]. Chin J Tissue Eng Res, 2024, 28(26): 4250-4256. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-XDKF202426023.htm [14] KEOHANE D M, WOODS T, O'CONNOR P, et al. Four men in a boat: ultra-endurance exercise alters the gut microbiome[J]. J Sci Med Sport, 2019, 22(9): 1059-1064. doi: 10.1016/j.jsams.2019.04.004 [15] ZHAO X, ZHANG Z, HU B, et al. Response of gut microbiota to metabolite changes induced by endurance exercise[J]. Front Microbiol, 2018, 9: 765. doi: 10.3389/fmicb.2018.00765 [16] GROSICKI G J, DURK R P, BAGLEY J R. Rapid gut microbiome changes in a world-class ultramarathon runner[J]. Physiol Rep, 2019, 7(24): e14313. [17] PASINI E, CORSETTI G, ASSANELLI D, et al. Effects of chronic exercise on gut microbiota and intestinal barrier in human with type 2 diabetes[J]. Minerva Med, 2019, 110(1): 3-11. [18] BUNPRAJUN T, YUAJIT C, NOITEM R, et al. Exhaustive exercise decreases renal organic anion transporter 3 function[J]. J Physiol Sci, 2019, 69(2): 245-251. doi: 10.1007/s12576-018-0641-5 [19] LUO B, XIANG D, NIEMAN D C, et al. The effects of moderate exercise on chronic stress-induced intestinal barrier dysfunction and antimicrobial defense[J]. Brain Behav Immun, 2014, 39: 99-106. doi: 10.1016/j.bbi.2013.11.013 [20] WANG G, ZHOU H, ZHANG L, et al. Effects of high-intensity interval training on gut microbiota profiles in 12 months' old ICR mice[J]. J Physiol Biochem, 2020, 76(4): 539-548. doi: 10.1007/s13105-020-00758-w [21] THARP G E. Tissue respiration changes in chronic exercise. Comparison with responses to other types of stresses[J]. Int Z Angew Physiol, 1971, 29(3): 195-202. [22] 中华人民共和国国家卫生和计划生育委员会. 学龄儿童青少年超重与肥胖筛查[J]. 中华人民共和国教育部公报, 2018, 56(8): 1-3. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHLX200402002.htmNational Health and Family Planning Commission of the PRC. Screening for overweight and obesity in school-age children and adolescents[J]. Bull Minist Educ PRC, 2018, 56(8): 1-3. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZHLX200402002.htm [23] MENG C, YUCHENG T, SHU L, et al. Effects of school-based high-intensity interval training on body composition, cardiorespiratory fitness and cardiometabolic markers in adolescent boys with obesity: a randomized controlled trial[J]. BMC Pediatr, 2022, 22(1): 112. doi: 10.1186/s12887-021-03079-z [24] CASTRO-PIÑERO J, ARTERO E G, ESPAÑA-ROMERO V, et al. Criterion-related validity of field-based fitness tests in youth: a systematic review[J]. Br J Sports Med, 2010, 44(13): 934-943. doi: 10.1136/bjsm.2009.058321 [25] 曹甍, 于丰源, 高榕蔓, 等. 高强度间歇训练运动对肥胖小学生身体健康影响[J]. 中国学校卫生, 2023, 44(12): 1863-1866. doi: 10.16835/j.cnki.1000-9817.2023.12.022CAO M, YU F Y, GAO R M, et al. Effects of high-intensity interval training exercise prescription on the physical health of obese primary school students[J]. Chin J Sch Health, 2023, 44(12): 1863-1866. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2023.12.022 [26] GABAY C, LAMACCHIA C, PALMER G. IL-1 pathways in inflammation and human diseases[J]. Nat Rev Rheumatol, 2010, 6(4): 232-241. doi: 10.1038/nrrheum.2010.4 [27] LEE H, CHEONG K A, KIM J Y, et al. IL-1 receptor antagonist reduced chemical-induced keratinocyte apoptosis through antagonism to IL-1α/IL-1β[J]. Biomol Ther (Seoul), 2018, 26(4): 417-423. doi: 10.4062/biomolther.2017.167 [28] 熊金龙, 阮志忠. 从慢性炎症角度探讨针灸治疗肥胖症的机制[J]. 基层中医药, 2023, 2(11): 87-91. https://www.cnki.com.cn/Article/CJFDTOTAL-JCEY202311022.htmXIONG J L, RUAN Z Z. Mechanism of acupuncture and moxibustion in treating obesity from the perspective of chronic infammation[J]. Basic Trad Chin Med, 2023, 2(11): 87-91. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-JCEY202311022.htm [29] ZHUANG Y, HUANG H, LIU S, et al. Resveratrol improves growth performance, intestinal morphology, and microbiota composition and metabolism in mice[J]. Front Microbiol, 2021, 12: 726878. doi: 10.3389/fmicb.2021.726878 [30] FREIDIN M B, STALTERI M A, WELLS P M, et al. An association between chronic widespread pain and the gut microbiome[J]. Rheumatology (Oxford), 2021, 60(8): 3727-3737. doi: 10.1093/rheumatology/keaa847 [31] 朱玲玲, 佘云, 余江毅, 等. 中药调控糖尿病肾脏疾病肾间质纤维化相关信号通路研究进展[J]. 中国实验方剂学杂志, 2024, 30(5): 213-225. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSFX202405026.htmZHU L L, SHE Y, YU J Y, et al. Signaling pathways related to renal interstitial fibrosis in diabetic kidney disease regulated bychinese medicine: a review[J]. Chin J Exp Tradit Med Formul, 2024, 30(5): 213-225. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZSFX202405026.htm [32] BÄCKHED F, DING H, WANG T, et al. The gut microbiota as an environmental factor that regulates fat storage[J]. Proc Natl Acad Sci USA, 2004, 101(44): 15718-15723. doi: 10.1073/pnas.0407076101 -







 下载:
下载: