Prevalence of non-alcoholic fatty liver disease and associated factors in overweight and obese children in Hohhot
-
摘要:
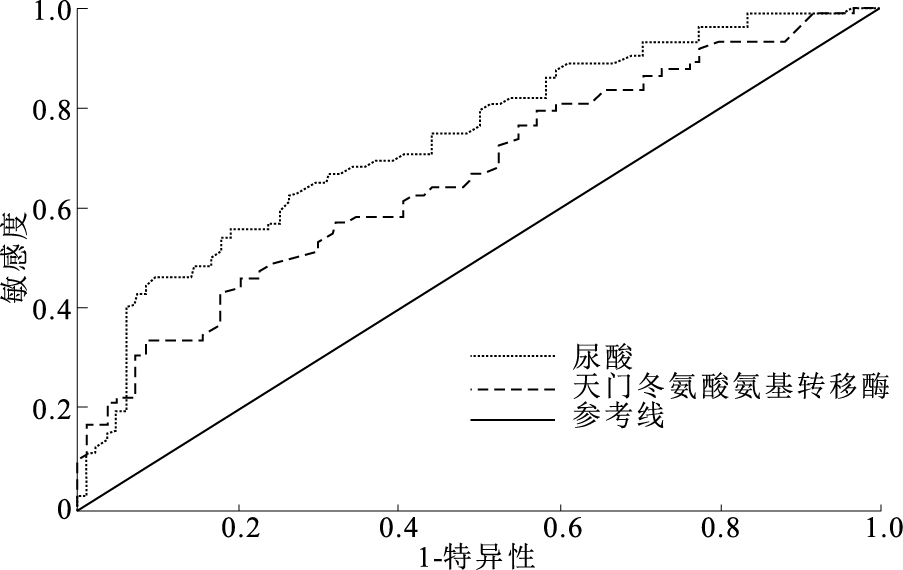
目的 探索呼和浩特市超重肥胖儿童非酒精性脂肪肝(NAFLD)患病现状及其相关因素,为制定健康教育计划和实施儿童NAFLD防治工作提供理论依据。 方法 于2022年8月28日至2023年3月5日,采用整群抽样方法从呼和浩特市4所小学抽取156名超重/肥胖儿童纳入研究;收集呼和浩特市超重/肥胖儿童基本信息,并抽取清晨空腹血液检测空腹血糖(GLU)、丙氨酸氨基转移酶(ALT)、天门冬氨酸氨基转移酶(AST)、γ谷氨酰基转移酶(γ-GGT)、尿酸(uric)、总胆固醇(TC)、甘油三酯(TG)、低密度脂蛋白(LDL)、高密度脂蛋白(HDL)、胰岛素(insulin)。采用t检验、χ2检验和Fisher确切概率法进行单因素分析,多因素分析采用Logistic回归分析并进行受试者特征曲线绘制。 结果 无NAFLD组和NAFLD组超重/肥胖儿童在年龄、腰围、臀围、GLU、ALT、AST、γ-GGT、uric和TG上差异均有统计学意义(U/t=1 070.0~2 164.0,P值均 < 0.05)。多因素分析中,AST升高和uric升高与NAFLD发生风险增高均相关[OR值(95%CI)分别为1.16(1.04~1.28),1.01(1.00~1.01),P值均 < 0.05]。受试者特征曲线下面积分别为AST=0.737,uric=0.665。 结论 呼和浩特地区超重/肥胖儿童NAFLD患病率较高,AST升高和uric升高可能会导致超重/肥胖儿童患NAFLD风险升高。应重点关注超重/肥胖儿童NAFLD的患病情况,建议在NAFLD的防治中同时降低BMI和uric水平,以达到更好的治疗效果。 Abstract:Objective To explore prevalence and associated factors of non-alcoholic fatty liver disease (NAFLD) in overweight and obese children in Hohhot City, so as to provide the oretical basis for developing health education plans and implementing prevention and treatment of NAFLD in children. Methods A total of 156 overweight and obese children was enrolled from 4 primary schools in Hohhot City using cluster sampling method during 28th Aug. 2022 to 5th Mar. 2023. Height and weight were measured and body mass index was calculated, and fasting blood was taken in the early morning for fasting blood glucose, alanine aminotransferase, aspartate aminotransferase. Single factor analysis was conducted using t-test, χ2 test and Fisher's exact probability method, while multivariate analysis was conducted using Logistic regression analysis and subject characteristic curves. Results The differences in age, waist circumference, hip circumference, fasting glucose, alanine aminotransferase, aspartate aminotransferase, gamma glutamyltransferase, uric acid, and triglyceride were statistically significant between the non-NAFLD and the NAFLD group (U/t=1 070.0-2 164.0, P < 0.05). Significant differences were observed in aspartate aminotransferase (AST) and uric acid levels (AST OR=1.16, 95%CI=1.04-1.28; uric OR=1.01, 95%CI=1.00-1.01, P < 0.05). The area under a receiver operating characteristic were 0.737 for aspartate aminotransferase and 0.665 for uric acid, respectively. Conclusions The prevalence of NAFLD is high in overweight/obese children in Hohhot, and both elevated aspartate aminotransferase and hyperuricemia could increase the risk of NAFLD in overweight/obese children. Special attention should be paid to the NAFLD in overweight and obese children. It is recommended to reduce both BMI and uric level in the prevention and treatment of NAFLD to achieve better treatment outcomes. -
Key words:
- Overweight /
- Obesity /
- Fatty liver /
- Prevalence /
- Regression analysis /
- Child /
- Minority groups
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 呼和浩特市6~14岁超重肥胖儿童NAFLD影响因素的单因素分析[M(P25,P75)]
Table 1. Univariate analysis of factors affecting NAFLD in overweight and obese children aged 6-14 years in Hohhot City[M(P25, P75)]
组别 人数 腰围/cm 臀围/cm GLU/(mmol·L-1)* ALT/(U·L-1) AST/(U·L-1) γ-GGT/(U·L-1) 非NAFLD 84 74(67.5,80.5) 86(78.0,94.0) 4.8±0.4 14.7(10.8,18.7) 21.2(17.6,24.8) 15.0(11.5,18.5) NAFLD 72 87(80.0,94.0) 97(89.5,104.5) 4.9±0.5 28.1(17.9,38.4) 24.1(19.1,29.1) 21(17.0,25.0) U/t值 1 258.0 1 458.5 -1.9 1 070.0 2 026.5 1 391.5 P值 <0.01 <0.01 0.06 <0.01 <0.01 <0.01 组别 人数 uric/ (μmol·L-1) TC/ (mmol·L-1)* TG/ (mmol·L-1) LDL/ (mmol·L-1)* HDL/ (mmol·L-1)* insulin/ pmol/L 非NAFLD组 84 350.5(305.0,396.0) 4.0±1.5 1.0(0.7,1.3) 2.4±0.5 1.3±0.3 119.5(76.8,162.1) NAFLD组 72 421.5(357.0,486.0) 4.1±0.8 1.2(0.7,1.7) 2.4±0.7 1.3±0.3 244.9(154.3,335.5) U/t值 1 593.5 -1.1 2 164.0 -0.7 0.4 1 318.5 P值 <0.01 0.27 <0.01 0.47 0.69 <0.01 注:*符合正态分布,采用(x ±s)表示。 表 2 呼和浩特市6~14岁超重肥胖儿童NAFLD影响因素的多因素Logistic回归分析(n=156)
Table 2. Multivariate Logistic regression analysis of the influencing factors of NAFLD in overweight and obese children aged 6-14 years in Hohhot City(n=156)
自变量 β值 标准误 OR(95%CI) P值 性别 0.08 0.49 1.08(0.41~2.85) 0.88 就诊年龄 -0.17 0.16 0.85(0.62~1.17) 0.31 腰围 0.02 0.05 1.02(0.93~1.13) 0.69 臀围 0.08 0.06 1.08(0.96~1.21) 0.19 GLU 0.56 0.61 1.75(0.53~5.72) 0.36 ALT 0.00 0.02 1.00(0.97~1.04) 0.83 AST 0.14 0.05 1.16(1.04~1.28) 0.01 γ-GGT 0.01 0.02 1.01(0.96~1.05) 0.81 uric 0.01 0.00 1.01(1.00~1.01) 0.03 TG 0.29 0.40 1.34(0.61~2.93) 0.47 insulin 0.00 0.00 1.00(1.00~1.01) 0.06 -
[1] DIEHL A M, DAY C. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis[J]. N Engl J Med, 2017, 377(21): 2063-2072. doi: 10.1056/NEJMra1503519 [2] 中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 实用肝脏病杂志, 2018, 21(2): 177-186. https://www.cnki.com.cn/Article/CJFDTOTAL-CRBX201805002.htmFatty Liver and Alcoholic Liver Disease Group of Hepatology Branch of Chinese Medical Association, Fatty Liver Expert Committee of Chinese Medical Association. Guidelines for the prevention and treatment of non-alcoholic fatty liver disease (2018 update)[J]. J Pract Liver Dis, 2018, 21(2): 177-186. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-CRBX201805002.htm [3] RIAZI K, AZHARI H, CHARETTE J H, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and Meta-analysis[J]. Lancet Gastroenterol Hepatol, 2022, 7(9): 851-861. doi: 10.1016/S2468-1253(22)00165-0 [4] ZHOU J, ZHOU F, WANG W, et al. Epidemiological features of NAF-LD from 1999 to 2018 in China[J]. Hepatology, 2020, 71(5): 1851-1864. doi: 10.1002/hep.31150 [5] ESTES C, ANSTEE Q M, ARIAS-LOSTE M T, et al. Modeling NAF-LD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030[J]. J Hepatol, 2018, 69(4): 896-904. doi: 10.1016/j.jhep.2018.05.036 [6] NOBILI V, ALISI A, VALENTI L, et al. NAFLD in children: new genes, new diagnostic modalities and new drugs[J]. Nat Rev Gastroenterol Hepatol, 2019, 16(9): 517-530. doi: 10.1038/s41575-019-0169-z [7] 吴敏, 陈联辉, 陈郎湖, 等. 心磷脂变化参与非酒精性脂肪性肝病相关线粒体功能障碍的发生和发展[J]. 中南大学学报(医学版), 2021, 46(6): 653-657. https://www.cnki.com.cn/Article/CJFDTOTAL-HNYD202106014.htmWU M, CHEN L H, CHEN L H, et al. Cardiolipin changes are involved in the onset and development of mitochondrial dysfunction associated with nonalcoholic fatty liver disease[J]. J Central South Univ (Med Edit), 2021, 46(6): 653-657. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-HNYD202106014.htm [8] 中华人民共和国国家卫生健康委员会. 学龄儿童青少年超重与肥胖筛查:WS/T 586—2018[S]. 2018-08-01. National Health Commission of the PRC. Screening for overweight and obesity in school-age children and adolescents: WS/T 586-2018[S]. 2018-08-01. (in Chinese) [9] 周雪莲, 傅君芬. 儿童非酒精性脂肪肝病诊断与治疗专家共识[J]. 中国实用儿科杂志, 2018, 33(7): 487-492. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSEK201807002.htmZHOU X L, FU J F. Expert consensus on diagnosis and treatment of non-alcoholic fatty liver disease in children[J]. Chin J Pract Paediatr, 2018, 33(7): 487-492. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZSEK201807002.htm [10] SHAUNAK M, BYRNE C D, DAVIS N, et al. Non-alcoholic fatty liver disease and childhood obesity[J]. Arch Dis Child, 2021, 106(1): 3-8. doi: 10.1136/archdischild-2019-318063 [11] 杨田, 张凯文, 高昇, 等. 内蒙古地区学生肥胖现状及影响因素分析[J]. 中国学校卫生, 2021, 42(4): 611-614. doi: 10.16835/j.cnki.1000-9817.2021.04.030YANG T, ZHANG K W, GAO S, et al. Analysis of obesity status and influencing factors of students in Inner Mongolia[J]. Chin J Sch Health, 2021, 42(4): 611-614. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2021.04.030 [12] 中华人民共和国国家卫生健康委员会. 中国居民营养与慢性病状况报告(2020年)[J]. 营养学报, 2020, 42(6): 521. https://www.cnki.com.cn/Article/CJFDTOTAL-CZSJ202114035.htmNational Health Commission of the PRC. Report on nutrition and chronic disease status of Chinese residents (2020)[J]. J Nutr, 2020, 42(6): 521. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-CZSJ202114035.htm [13] 陈新春, 寇永妹, 刘晓璐, 等. 唐山市7~14岁肥胖儿童非酒精性脂肪肝流行现状及危险因素初步分析[J]. 中国儿童保健杂志, 2021, 29(6): 669-673. https://www.cnki.com.cn/Article/CJFDTOTAL-ERTO202106023.htmCHEN X C, KOU Y M, LIU X L, et al. Preliminary analysis of the prevalence and risk factors of non-alcoholic fatty liver disease in obese children aged 7-14 years in Tangshan City[J]. Chin J Child Health, 2021, 29(6): 669-673. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ERTO202106023.htm [14] 蒋雪, 高健, 洪泽, 等. 维生素D治疗肥胖合并非酒精性脂肪肝儿童的临床研究[J]. 中国儿童保健杂志, 2022, 30(9): 970-974. https://www.cnki.com.cn/Article/CJFDTOTAL-ERTO202209009.htmJIANG X, GAO J, HONG Z, et al. Clinical study of vitamin D treatment in children with obesity combined with non-alcoholic fatty liver disease[J]. Chin J Child Health, 2022, 30(9): 970-974. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ERTO202209009.htm [15] 王雨, 杨志然, 陈润花. 中国儿童非酒精性脂肪性肝病患病率的Meta分析[J]. 中国儿童保健杂志, 2022, 30(7): 764-769. https://www.cnki.com.cn/Article/CJFDTOTAL-ERTO202207015.htmWANG Y, YANG Z R, CHEN R H. Meta-analysis of the prevalence of non-alcoholic fatty liver disease in Chinese children[J]. Chin J Child Health, 2022, 30(7): 764-769. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ERTO202207015.htm [16] ANDERSON E L, HOWE L D, JONES H E, et al. The prevalence of non-alcoholic fatty liver disease in children and adolescents: a systematic review and Meta-analysis[J]. PLoS One, 2015, 10(10): e0140908. [17] 李东丹, 闫洁, 王美辰, 等. 非酒精性脂肪性肝病肥胖儿童人体成分及其影响因素分析[J]. 中国实用儿科杂志, 2023, 38(7): 525-529. https://www.cnki.com.cn/Article/CJFDTOTAL-ZSEK202307010.htmLI D D, YAN J, WANG M C, et al. Analysis of body composition and its influencing factors in obese children with non-alcoholic fatty liver disease[J]. Chin J Pract Paediatr, 2023, 38(7): 525-529. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZSEK202307010.htm [18] 杨青华, 代东伶. 儿童NAFLD的危险因素分析[C]//中国中西医结合学会儿科专业委员会. 第二十三次全国儿科中西医结合学术会议资料汇编. 深圳: 深圳市儿童医院, 2019.YANG Q H, DAI D L. Analysis of risk factors for NAFLD in children[C]//Pediatrics Committee of the Chinese Society of Integrative Medicine. Compilation of materials of the 23rd National Academic Conference on Integrative Medicine in Paediatrics. Shenzhen: Shenzhen Children's Hospital, 2019. (in Chinese) [19] SUN Q, ZHANG T, MANJI L, et al. Association between serum uric acid and non-alcoholic fatty liver disease: an updated systematic review and Meta-analysis[J]. Clin Epidemiol, 2023, 15: 683-693. [20] LANASPA M A, SANCHEZ-LOZADA L G, CHOI Y J, et al. Uric acid induces hepatic steatosis by generation of mitochondrial oxidative stress: potential role in fructose-dependent and-independent fatty liver[J]. J Biol Chem, 2012, 287(48): 40732-40744. -







 下载:
下载: