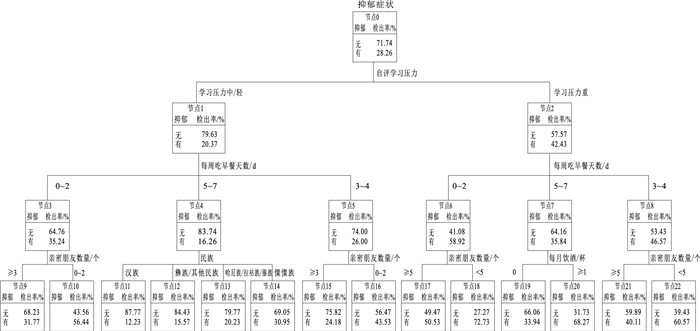
Decision tree model of depressive symptoms among first-grade students from multi-ethnic middle schools in Yunnan Province
-
摘要:
目的 了解云南省多民族初中学生抑郁症状发生情况及其预测因素,为学校有针对性地开展心理健康教育提供参考依据。 方法 于2022年10—12月,采用整群随机抽样方法在云南省11个少数民族地区选取23所中学的8 500名初一年级学生,使用问卷调查收集中学生人口统计学和生活行为方式数据,采用儿童抑郁量表(CDI)评估抑郁症状。单因素分析使用χ2检验比较不同人口学变量的初一年级学生抑郁症状检出率,采用卡方自动交互检测法(CHAID)建立中学生抑郁症状决策树模型。 结果 云南省多民族初一年级学生抑郁症状检出率为28.26%。抑郁症状决策树的第1层是自评学习压力(χ2=469.08),第2层是早餐行为(中/轻度学习压力:χ2=155.49;重度学习压力:χ2=105.24),第3层是亲密朋友数量(中/轻度学习压力,每周吃早餐0~2 d:χ2=23.15;中/轻度学习压力,每周吃早餐3~4 d:χ2=14.99;重度学习压力,每周吃早餐0~2 d:χ2=29.26;重度学习压力,每周吃早餐3~4 d:χ2=20.15)、民族(χ2=78.22)和饮酒(χ2=50.36)(P值均<0.01)。 结论 学习压力、早餐行为、亲密朋友数量、饮酒和民族是云南省多民族中学生抑郁症状的预测因子。学校应有针对性地制定抑郁症状防控策略,减少中学生抑郁症状的发生。 Abstract:Objective To understand the occurrence and predictive factors of depressive symptoms among multi-ethnic middle school students in Yunnan Province, so as to provide a referential framework for schools to carry out targeted mental health education. Methods From October to December 2022, 8 500 first-grade students from 23 middle schools were selected from 11 minority areas in Yunnan Province by cluster random sampling method. Demographic information and data relating to the students' lifestyles were collected by questionnaire, and the Children's Depression Inventory (CDI) was used to evaluate depressive symptoms. Chi-square test was performed to compare differences in the detection rate of depressive symptoms among first-grade middle school students for univariate analysis. A decision tree model of depressive symptoms in middle school students was established by using the Chi-squared automatic interaction detector (CHAID). Results The detection rate of depressive symptoms among first-grade students from multi-ethnic middle schools in Yunnan Province was 28.26%. The decision tree model of depressive symptoms was academic stress (χ2=469.08) at the first level, breakfast behaviors (low/moderate academic stress: χ2=155.49; severe academic stress: χ2=105.24) at the second level, and the number of close friends (low/moderate academic stress and consuming breakfast 0-2 days weekly: χ2=23.15; low/moderate academic stress and consuming breakfast 3-4 days weekly: χ2=14.99; severe academic stress and consuming breakfast 0-2 days weekly: χ2=29.26; severe academic stress and consuming breakfast 3-4 days weekly: χ2=20.15), ethnicity (χ2=78.22) and drinking (χ2=50.36) at the third level (P<0.01). Conclusions The study identifies academic stress, breakfast behaviors, number of close friends, drinking and ethnicity as predictive factors of depressive symptoms among multi-ethnic middle school students in Yunnan Province. Schools should develop targeted strategies for preventing and managing depressive symptoms in middle school students, so as to reduce their occurrence. -
Key words:
- Depression /
- Mental health /
- Decision trees /
- Students /
- Minority groups
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 云南省不同人口学特征多民族初一年级学生抑郁症状检出率比较
Table 1. Comparison of detection rates of depressive symptoms among first-grade students from multi-ethnic middle schools with different demographic characteristics in Yunnan Province
组别 选项 人数 抑郁症状 χ2值 P值 组别 选项 人数 抑郁症状 χ2值 P值 年龄/岁 12 3 698 987(26.69) 36.45 <0.01 父亲文化程度 小学未毕业或没上过学 1 084 368(33.95) 24.70 <0.01 13 4 259 1 204(28.27) 小学 1 956 558(28.53) 14 461 174(37.74) 初中 3 931 1 067(27.14) 15 82 37(45.12) 高中/中专 1 056 297(28.13) 性别 男 4 184 1 069(25.55) 29.83 <0.01 大专及以上 473 112(23.68) 女 4 316 1 333(30.89) 母亲文化程度 小学未毕业或没上过学 1 700 559(32.88) 30.44 <0.01 民族 汉族 3 856 947(24.56) 113.47 <0.01 小学 2 045 588(28.75) 哈尼族 1 585 465(29.34) 初中 3 472 902(25.98) 彝族 1 379 369(26.76) 高中/中专 872 253(29.01) 傈僳族 601 256(42.60) 大专及以上 411 100(24.33) 拉祜族 254 101(39.76) 父亲职业 公职人员b 4 173 1 174(28.13) 14.46 0.01 傣族 235 83(35.32) 工人 502 128(25.50) 其他民族 590 181(30.68) 公司职员 1 798 520(28.92) 家庭居住地 农村 6 358 1 824(28.69) 2.30 0.13 商人 659 156(23.67) 城镇 2 142 578(26.98) 农民 269 80(29.74) 独生子女 是 1 256 395(31.45) 7.40 0.01 其他 1 099 344(31.30) 否 7 244 2 007(27.71) 母亲职业 公职人员b 4 660 1 328(28.50) 14.59 0.01 家庭类型 双亲 6 878 1 825(26.53) 54.91 <0.01 工人 409 94(22.98) 单亲 862 300(34.80) 公司职员 1 047 299(28.56) 组合a 617 219(35.49) 商人 758 192(25.33) 其他 143 58(40.56) 农民 324 85(26.23) 自评家庭经济状况 差 1 127 498(44.19) 169.88 <0.01 其他 1 302 404(31.03) 中 6 000 1 590(26.50) 好 1 373 314(22.87) 注:()内数字为检出率/%;a有继父或继母,b为公务员及事业单位人员。 表 2 云南省多民族初一年级学生抑郁症状单因素分析
Table 2. Univariate analysis of depressive symptoms among first-grade students from multi-ethnic middle schools in Yunnan Province
组别 选项 人数 抑郁症状 χ2值 P值 组别 选项 人数 抑郁症状 χ2值 P值 家庭变故 是 1 061 389(36.66) 42.24 <0.01 每周吃夜宵天数/d 0 2 217 572(25.80) 25.78 <0.01 否 7 439 2 013(27.06) 1~2 2 976 800(26.88) 住院经历 是 1 377 488(35.44) 41.79 <0.01 3~4 1 640 494(30.12) 否 7 123 1 914(26.87) 5~6 667 205(30.73) 新型冠状病毒感染疫情影响学习 是 3 362 1 092(32.48) 48.90 <0.01 7 1 000 331(33.10) 否 5 138 1 310(25.50) 每周吃西式快餐频率/d 0 6 122 1 708(27.90) 21.98 <0.01 抑郁症家族史 是 192 94(48.96) 41.52 <0.01 1~2 2 027 560(27.63) 否 8 308 2 308(27.78) 3~4 243 85(34.98) 学习日视屏时间/h <1 4 862 1 255(25.81) 95.10 <0.01 5~6 44 19(43.18) 1~<2 1 765 503(28.50) ≥7 64 30(46.88) 2~<3 982 308(31.36) 每周吃中式快餐频率/d 0 5 594 1 493(26.69) 41.44 <0.01 3~<4 433 123(28.41) 1~2 2 128 619(29.09) 4~<5 168 74(44.05) 3~4 479 181(37.79) ≥5 290 139(47.93) 5~6 146 47(32.19) 休息日视屏时间/h <1 1 790 467(26.09) 140.86 <0.01 ≥7 153 62(40.52) 1~<2 2 334 584(25.02) 每周吃外卖快餐频率/d 0 6 835 1 829(26.76) 68.94 <0.01 2~<3 1 968 499(25.36) 1~2 1 151 360(31.28) 3~<4 1 085 319(29.40) 3~4 317 117(36.91) 4~<5 480 157(32.71) 5~6 113 49(43.36) ≥5 843 376(44.60) ≥7 84 47(55.95) 留守经历 是 2 334 856(36.68) 112.42 <0.01 每周喝含糖饮料频率/d 0 2 085 548(26.28) 104.50 <0.01 否 6 166 1 546(25.07) 1~2 3 837 983(25.62) 每天吸烟/支 0 8 239 2 243(27.22) 168.13 <0.01 3~4 1 412 402(28.47) 1~2 135 64(47.41) 5~6 577 215(37.26) 3~4 46 33(71.74) ≥7 589 254(43.12) 5~6 28 20(71.43) 每周吃零食频率/d 0 1 195 349(29.21) 62.84 <0.01 ≥7 52 42(80.77) 1~2 3 734 948(25.39) 自评学习压力 重 3 040 1 290(42.43) 469.39 <0.01 3~4 2 011 546(27.15) 中 5 190 1 053(20.29) 5~6 845 291(34.44) 轻 270 59(21.85) ≥7 715 268(37.48) 亲密朋友数量/个 0~2 945 437(46.24) 193.19 <0.01 每月饮酒/杯 0 8 079 2 169(26.85) 165.24 <0.01 3~4 1 361 427(31.37) 1~2 231 119(51.52) ≥5 6 194 1 538(24.83) 3~4 73 46(63.01) 每周吃早餐天数/d 0~2 1 329 613(46.12) 318.98 <0.01 5~6 43 23(53.49) 3~4 1 458 493(33.81) ≥7 74 45(60.81) 5~7 5 713 1 296(22.69) 注:()内数字为检出率/%。 -
[1] SHOREY S, NG E D, WONG C H J. Global prevalence of depression and elevated depressive symptoms among adolescents: a systematic review and Meta-analysis[J]. Br J Clin Psychol, 2022, 61(2): 287-305. doi: 10.1111/bjc.12333 [2] MALHI G S, MANN J J. Depression[J]. Lancet, 2018, 392(10161): 2299-2312. doi: 10.1016/S0140-6736(18)31948-2 [3] 刘福荣, 宋晓琴, 尚小平, 等. 中学生抑郁症状检出率的Meta分析[J]. 中国心理卫生杂志, 2020, 34(2): 123-128. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXWS202002009.htmLIU F R, SONG X Q, SHANG X P, et al. A Meta-analysis of detection rate of depression symptoms among middle school students[J]. Chin Mental Health J, 2020, 34(2): 123-128. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZXWS202002009.htm [4] ZHANG X, YAN Y, YE Z, et al. Descriptive analysis of depression among adolescents in Huangshi, China[J]. BMC Psychiatry, 2023, 23(1): 176. doi: 10.1186/s12888-023-04682-3 [5] 徐涛, 周县委, 张天成, 等. 中国中学生抑郁症状危险因素的Meta分析[J]. 现代预防医学, 2022, 49(5): 814-818, 844. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF202205010.htmXU T, ZHOU X W, ZHANG T C, et al. Risk factors of depression symptom among Chinese middle school students: a Meta-analysis[J]. Mod Prev Med, 2022, 49(5): 814-818, 844. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF202205010.htm [6] 张桂杰, 王小灿, 邢维康, 等. 基于决策树分类算法的心理测评模型研究[J]. 吉林师范大学学报, 2023, 44(4): 123-130. https://www.cnki.com.cn/Article/CJFDTOTAL-SLXK202304018.htmZHANG G J, WANG X C, XING W K, et al. Research on psychological assessment model based on decision tree classification algorithm[J]. J Jilin Normal Univ, 2023, 44(4): 123-130. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-SLXK202304018.htm [7] 徐洪吕, 万宇辉, 张诗晨, 等. 青少年抑郁症状与外卖快餐碳酸饮料消费相关性分析[J]. 中国学校卫生, 2019, 40(4): 538-541, 545. doi: 10.16835/j.cnki.1000-9817.2019.04.017XU H L, WAN Y H, ZHANG S C, et al. Interaction effects of co-consumption of takeaway fast foods and sodas on depressive symptom in Chinese adolescents[J]. Chin J Sch Health, 2019, 40(4): 538-541, 545. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2019.04.017 [8] 柳之啸, 李京, 王玉, 等. 中文版儿童抑郁量表的结构验证及测量等值[J]. 中国临床心理学杂志, 2019, 27(6): 1172-1176. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLCY201906020.htmLIU Z X, LI J, WANG Y, et al. Structural verification and measurement invariance of Chinese version of Children's Depression Inventory[J]. Chin J Clin Psychol, 2019, 27(6): 1172-1176. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-ZLCY201906020.htm [9] 洪忻, 李解权, 梁亚琼, 等. 儿童抑郁量表中文版在中学生中的信效度分析[J]. 中国学校卫生, 2012, 33(10): 1182-1185. https://www.cnki.com.cn/Article/CJFDTOTAL-XIWS201210010.htmHONG X, LI J Q, LIANG Y Q, et al. Reliability and validity of the Chinese version of Children' s Depression Inventory[J]. Chin J Sch Health, 2012, 33(10): 1182-1185. (in Chinese) https://www.cnki.com.cn/Article/CJFDTOTAL-XIWS201210010.htm [10] ZHANG X, GAO F, KANG Z, et al. Perceived academic stress and depression: the mediation role of mobile phone addiction and sleep quality[J]. Front Public Health, 2022, 10: 760387. doi: 10.3389/fpubh.2022.760387 [11] REN Z, ZHOU G, WANG Q, et al. Associations of family relationships and negative life events with depressive symptoms among Chinese adolescents: a cross-sectional study[J]. PLoS One, 2019, 14(7): e0219939. doi: 10.1371/journal.pone.0219939 [12] ZENG X, CHEN Y, ZHANG Q, et al. Multidimensional self-rating biological rhythm disorder and its association with depression and anxiety symptoms among adolescents aged 11-23 years: a school-based cross-sectional study from China[J]. BMC Psychiatry, 2022, 22(1): 700. doi: 10.1186/s12888-022-04354-8 [13] JAYANTHI P, THIRUNAVUKARASU M, RAJKUMAR R. Academic stress and depression among adolescents: a cross-sectional study[J]. Indian Pediat, 2015, 52(3): 217-219. doi: 10.1007/s13312-015-0609-y [14] ALI N M, NOWSHAD N A, MANSOOR K M, et al. Perceived academic and psychological stress among adolescents in United Arab Emirates: role of gender, age, depression, and high expectation of parents[J]. Psychiatr Danub, 2019, 31(Suppl 3): 331-337. [15] SCHMIDT H D, DUMAN R S. The role of neurotrophic factors in adult hippocampal neurogenesis, antidepressant treatments and animal models of depressive-like behavior[J]. Behav Pharmacol, 2007, 18(5-6): 391-418. doi: 10.1097/FBP.0b013e3282ee2aa8 [16] YANG L, ZHAO Y, WANG Y, et al. The effects of psychological stress on depression[J]. Curr Neuropharmacol, 2015, 13(4): 494-504. doi: 10.2174/1570159X1304150831150507 [17] ZAHEDI H, DJALALINIA S, SADEGHI O, et al. Breakfast consumption and mental health: a systematic review and Meta-analysis of observational studies[J]. Nutr Neurosci, 2022, 25(6): 1250-1264. doi: 10.1080/1028415X.2020.1853411 [18] PENGPID S, PELTZER K. Skipping breakfast and its association with health risk behaviour and mental health among university students in 28 countries[J]. Diabetes Metab Syndr Obes, 2020, 13: 2889-2897. doi: 10.2147/DMSO.S241670 [19] ZURAIKAT F M, WOOD R A, BARRAGÁN R, et al. Sleep and diet: mounting evidence of a cyclical relationship[J]. Annu Rev Nutr, 2021, 41: 309-332. doi: 10.1146/annurev-nutr-120420-021719 [20] JENKINS T A, NGUYEN J C, POLGLAZE K E, et al. Influence of tryptophan and serotonin on mood and cognition with a possible role of the gut-brain axis[J]. Nutrients, 2016, 8(1): 56. doi: 10.3390/nu8010056 [21] GIMÉNEZ-LEGARRE N, MIGUEL-BERGES M L, FLORES-BARRANTES P, et al. Breakfast characteristics and its association with daily micronutrients intake in children and adolescents: a systematic review and Meta-analysis[J]. Nutrients, 2020, 12(10): 3201. doi: 10.3390/nu12103201 [22] WANG J, UM P, DICKERMAN B A, et al. Zinc, magnesium, selenium and depression: a review of the evidence, potential mechanisms and implications[J]. Nutrients, 2018, 10(5): 584. doi: 10.3390/nu10050584 [23] BOKSZCZANIN A, PALACE M, BROWN W, et al. Depression, perceived risk of COVID-19, loneliness, and perceived social support from friends among university students in Poland, UK, and India[J]. Psychol Res Behav Manage, 2023, 16: 651-663. doi: 10.2147/PRBM.S380318 [24] KANG M, MIN A, MIN H. Predicting multicultural adolescents' depression in South Korea: roles of ego-resilience and social support[J]. J Pediatr Nurs, 2022, 65: e93-e98. doi: 10.1016/j.pedn.2022.03.012 [25] ACHTERBERGH L, PITMAN A, BIRKEN M, et al. The experience of loneliness among young people with depression: a qualitative Meta-synthesis of the literature[J]. BMC Psychiatry, 2020, 20(1): 415. doi: 10.1186/s12888-020-02818-3 [26] GRIFFITHS K M, CRISP D A, BARNEY L, et al. Seeking help for depression from family and friends: a qualitative analysis of perceived advantages and disadvantages[J]. BMC Psychiatry, 2011, 11: 196. doi: 10.1186/1471-244X-11-196 [27] CHOW M S C, POON S H L, LUI K L, et al. Alcohol consumption and depression among university students and their perception of alcohol use[J]. East Asian Arch Psychiatry, 2021, 31(4): 87-96. doi: 10.12809/eaap20108 [28] LINA-JOLIEN P, ROCÍO G J, MIQUEL R, et al. Moderate alcohol consumption and depression prevention: a critical review[J]. Actas Esp Psiquiatr, 2022, 50(3): 126-133. [29] RICHARDSON H N, LEE S Y, O'DELL L E, et al. Alcohol self-administration acutely stimulates the hypothalamic-pituitary-adrenal axis, but alcohol dependence leads to a dampened neuroendocrine state[J]. Eur J Neurosci, 2008, 28(8): 1641-1653. doi: 10.1111/j.1460-9568.2008.06455.x [30] FLORES-BONILLA A, RICHARDSON H N. Sex differences in the neurobiology of alcohol use disorder[J]. Alcohol Res, 2020, 40(2): 4. [31] ZHANG X, HUANG R, HO S Y, et al. Alcohol drinking, especially light drinking, and depressive symptoms in adolescents[J]. Drug Alcohol Depend, 2021, 227: 108932. doi: 10.1016/j.drugalcdep.2021.108932 -







 下载:
下载: