Association between the risk of tuberculosis outbreak in schools and the visit interval of index cases
-
摘要:
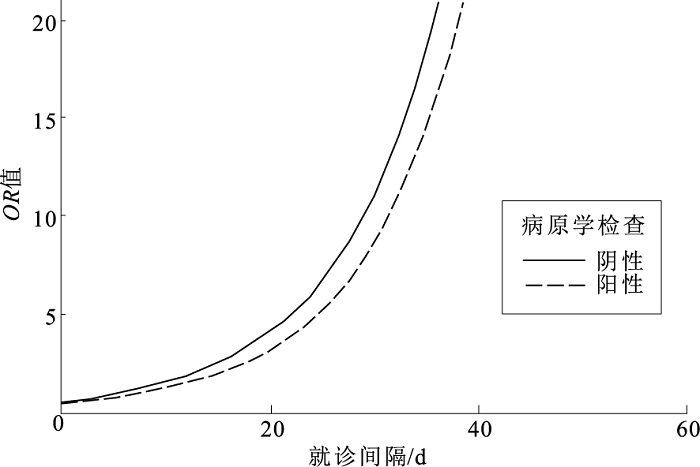
目的 分析学校肺结核疫情风险与指示病例就诊间隔的关系, 为公共卫生部门预判肺结核疫情聚集风险和制定干预措施提供科学依据。 方法 以2015年1月至2022年12月期间, 苏州市学校肺结核疫情630例指示病例为研究对象, 收集其人口统计学、就诊史、病原学诊断以及发现方式等资料。采用限制性立方样条(RCS), 非条件Logistic回归和受试者工作特征曲线(ROC曲线)进行统计学分析。 结果 RCS拟合曲线显示, 当病原学阴性患者就诊间隔>5.79 d, 或病原学阳性患者就诊间隔>8.37 d时, 肺结核疫情风险呈线性增加。调整性别、年龄和病原学检查后, 指示病例就诊间隔每延长1 d, 疫情发生高风险的OR值(95%CI)为1.10(1.07~1.13)(P<0.05)。按就诊间隔三分位分析, 与就诊间隔<14 d相比, 就诊间隔在14~<28 d和≥28 d的学校肺结核发生高风险疫情的OR值(95%CI)分别为10.32(3.04~35.10)和82.58(28.42~239.95)(P值均<0.01), 呈就诊间隔延长, 疫情风险上升趋势。通过ROC曲线分析, 预测学校肺结核疫情高风险的最佳阈值为23.5 d, 曲线下面积为0.93(95%CI=0.89~0.98)。 结论 指示病例就诊间隔延长是学校肺结核高风险疫情的良好预警指标, 可作为疫情早期干预和风险控制的关键考量。 Abstract:Objective To analyze the relationship between the risk of tuberculosis outbreaks in schools and the visit interval of index cases, so as to provide a scientific reference for predicting the risks of tuberculosis outbreak and making preventive measures. Methods A total of 630 index cases from school tuberculosis outbreaks were studied during January, 2015 to December, 2022. Data on demographics, consultation history, etiological diagnosis, and methods of detection were collected. Restricted Cubic Splines (RCS), unconditional Logistic regression, and the receiver operating characteristic curve (ROC curve) were used for analysis. Results The RCS fitted curve showed that the risk of a tuberculosis outbreak linearly increased when the consultation interval for etiologically negative patients exceeded 5.79 days, or for etiologically positive patients exceeded 8.37 days. After multi-factor adjustment, for every additional day in the visit interval of the index case, the odds ratio (OR) value for a high-risk outbreak was 1.10 (95%CI=1.07-1.13)(P < 0.05). When analyzed by tertiles of visit intervals, compared to an interval of < 14 days, the OR values (95%CI) for high-risk outbreaks in schools with intervals of 14- < 28 days and ≥28 days were 10.32(3.04-35.10) and 82.58(28.42-239.95), respectively(P < 0.01), indicating a trend of increasing outbreak risk with longer visit intervals. Based on the ROC curve analysis, the optimal threshold for predicting a high-risk school tuberculosis outbreak was 23.5 days, with an area under the curve (AUC) of 0.93 (95%CI=0.89-0.98). Conclusion An extended visit interval of index cases is a good early warning indicator for high-risk tuberculosis outbreaks in schools and could be considered a key factor in early intervention and risk control strategies. -
Key words:
- Tuberculosis, pulmonary /
- Disease outbreaks /
- Case reports /
- Ambulatory care /
- Students
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 不同特征指示病例构成在低风险疫情区与高风险疫情区组间比较
Table 1. Comparison of different characteristic compositions of indicating cases between low risk epidemic areas and high risk epidemic areas
特征 选项 低风险疫情(n=578) 高风险疫情(n=52) χ2值 P值 性别 男 346(59.86) 35(67.31) 1.11 0.29 女 232(40.14) 17(32.69) 学校类别 幼儿园/早教机构 18(3.11) 0 7.32 0.20 小学 50(8.65) 0 初中 78(13.49) 9(17.31) 高中 122(21.11) 12(23.08) 职业院校/中专 216(37.37) 23(44.23) 大学 94(16.26) 8(15.38) 人员类别 教职工 61(10.55) 3(5.77) 1.20 0.27 学生 517(89.45) 49(94.23) 病原学检查 阴性 298(51.56) 16(30.77) 8.25 <0.01 阳性 280(48.44) 36(69.23) 发现方式 因症就诊 475(82.18) 42(80.77) 0.15 0.93 主动筛查 17(2.94) 2(3.85) 健康体检 86(14.88) 8(15.38) 注: ()内数字为构成比/%。 表 2 就诊间隔预测肺结核高风险疫情效能评估(n=630)
Table 2. Evaluation of the efficacy of visit intervals in predicting high-risk tuberculosis outbreaks(n=630)
特征 阈值/d 灵敏度/% 特异度/% 阳性预测值/% 阴性预测值/% AUC(95%CI) 就诊间隔 23.5 82.69 88.93 98.28 40.19 0.93(0.89~0.98) 病原学阳性就诊间隔 29.5 77.78 92.86 97.01 58.33 0.92(0.86~0.98) 病原学阴性就诊间隔 15.5 93.75 80.20 99.58 20.27 0.94(0.89~0.99) -
[1] SU W, RUAN Y, LI T, et al. Epidemiological characteristics of rifampicin-resistant tuberculosis in students: China, 2015-2019[J]. China CDC Wkly, 2021, 3(26): 549-552. doi: 10.46234/ccdcw2021.142 [2] DU C R, WANG S C, YU M C, et al. Effect of ventilation improvement during a tuberculosis outbreak in underventilated university buildings[J]. Indoor Air, 2020, 30(3): 422-432. doi: 10.1111/ina.12639 [3] HOU J, PANG Y, YANG X, et al. Outbreak of mycobacterium tuberculosis Beijing strain in a high school in Yunnan, China[J]. Am J Trop Med Hyg, 2020, 102(4): 728-730. doi: 10.4269/ajtmh.19-0533 [4] BAO H, LIU K, WU Z, et al. Tuberculosis outbreaks among students in mainland China: a systematic review and Meta-analysis[J]. BMC Infect Dis, 2019, 19(1): 972. doi: 10.1186/s12879-019-4573-3 [5] 中华人民共和国国家卫生和计划生育委员会. 肺结核诊断标准: WS 288-2017[J]. 新发传染病电子杂志, 2018, 3(1): 59-61.National Health and Family Planning Commission of the PRC. Diagnostic for pulmonary tuberculosis standard: WS 288-2017[J]. Chin J Antituberc, 2018, 3(1): 59-61. (in Chinese) [6] 张晓龙, 王斐娴, 傅颖, 等. 2015-2017年苏州市学校结核病聚集性疫情调查[J]. 现代预防医学, 2019, 46(14): 2634-2637.ZHANG X L, WANG F X, FU X, et al. Epidemic analysis of school tuberculosis outbreak in Suzhou City between 2015 and 2017[J]. Mod Prev Med, 2019, 46(14): 2634-2637. (in Chinese) [7] National Tuberculosis Controllers Association, Centers for Disease Control and Prevention (CDC). Guidelines for the investigation of contacts of persons with infectious tuberculosis. Recommendations from the National Tuberculosis Controllers Association and CDC[J]. MMWR Recomm Rep, 2005, 54(RR-15): 1-47. [8] 姜洪波, 路希维. 重视学校结核病暴发的应用性研究[J]. 结核病与肺部健康杂志, 2015, 4(1): 5-8.JIANG H B, LU X W. Emphasis was placed on the application study of tuberculosis outbreak in schools[J]. J Tuberc Lung Health, 2015, 4(1): 5-8. (in Chinese) [9] TEO A K J, SINGH S R, PREM K, et al. Duration and determinants of delayed tuberculosis diagnosis and treatment in high-burden countries: a mixed-methods systematic review and Meta-analysis[J]. Respir Res, 2021, 22(1): 251. doi: 10.1186/s12931-021-01841-6 [10] KO Y, MIN J, KIM H W, et al. Time delays and risk factors in the management of patients with active pulmonary tuberculosis: nationwide cohort study[J]. Sci Rep, 2022, 12(1): 11355. doi: 10.1038/s41598-022-15264-w [11] CINQUETTI S, DALMANZIO M, ROS E, et al. High rate of transmission in a pulmonary tuberculosis outbreak in a primary school, north-eastern Italy, 2019[J]. Eur Surv, 2019, 24(24): 1900332. [12] OBSA M S, DAGA W B, WOSENE N G, et al. Treatment seeking delay and associated factors among tuberculosis patients attending health facility in Ethiopia from 2000 to 2020: a systematic review and Meta analysis[J]. PLoS One, 2021, 16(7): e0253746. doi: 10.1371/journal.pone.0253746 [13] 龚德华, 谭文倩, 黄娟, 等. 2011-2020年湖南省学生肺结核患者发现延误及其影响因素分析[J]. 中国防痨杂志, 2023, 45(3): 271-278.GONG D H, TAN W Q, HUANG J, et al. Analysis of the detection delay and influencing factors of student with pulmonary tuberculosis in Hunan from 2011 to 2020[J]. Chin J Antituberc, 2023, 45(3): 271-278. (in Chinese) [14] 谢祎, 韩晶, 于维莉, 等. 天津市肺结核患者短程督导治疗期抗结核治疗效果及死亡影响因素[J]. 中国公共卫生, 2020, 36(1): 126-129.XIE Y, HAN J, YU W L, et al. Treatment effect and risk factors of mortality among pulmonary tuberculosis patients with directly observed treatment short-course in Tianjin City[J]. Chin J Public Health, 2020, 36(1): 126-129. (in Chinese) [15] PARSONS L M, SOMOSKÖVI A, GUTIERREZ C, et al. Laboratory diagnosis of tuberculosis in resource-poor countries: challenges and opportunities[J]. Clin Microbiol Rev, 2011, 24(2): 314-350. doi: 10.1128/CMR.00059-10 [16] 律彤, 杨蕊, 陈金瓯, 等. 云南省病原学阳性肺结核患者总延迟变化趋势[J]. 中华疾病控制杂志, 2022, 26(5): 547-553.LYU T, YANG R, CHEN J O, et al. Analysis of the trend of total delay among pulmonary tuberculosis patients with positive etiology in Yunnan Province[J]. Chin J Dis Control Prev, 2022, 26(5): 547-553. (in Chinese) [17] UPLEKAR M, WEIL D, LONNROTH K, et al. WHO's new end TB strategy[J]. Lancet, 2015, 385(9979): 1799-1801. doi: 10.1016/S0140-6736(15)60570-0 -







 下载:
下载: