Research progress on burden and etiological mechanism of mental health as the core comorbidity in children and adolescents
-
摘要: 儿童青少年精神健康问题发生率逐渐上升,已成为关系国家和民族未来的重要公共卫生问题;但精神疾病很少独立存在,共病经常发生,给个人、家庭和社会带来巨大的危害和负担。研究综述了儿童青少年精神疾病为核心的共病流行状况及其不同类型的特征与表现,阐述其主要的共病病因机制,并提出了未来的研究方向设想。Abstract: The prevalence of mental health problems in children and adolescents has been gradually increasing, which has become an important public health problem related to the future of the country and the nation. However, mental disorder rarely exists independently, and comorbidity often occurs, which brings great harm and burden to individuals, families and society. This study introduces the prevalence, burden, characteristics and manifestations of different types of comorbidity with mental disorders as the core. Then it explaines the main causes and mechanisms of comorbidity, and proposes future research directions.
-
Key words:
- Comorbidity /
- Mental health /
- Cost of illness /
- Child /
- Adolescent
1) 利益冲突声明 所有作者声明无利益冲突。 -
儿童青少年精神疾病的日益流行引发了对其预防和管理策略的广泛研究[1-2],但精神疾病很少独立存在,多病/共病(通常定义为同一个体存在≥2种的疾病)经常发生[3]。与单一问题相比,共发性精神健康问题对儿童身心健康、学业成就和社会功能造成更消极的影响,也会增加物质滥用、违法犯罪甚至自杀等一系列不良发展结果的风险[4-5]。虽然精神健康共病给个人、家庭、卫生保健系统和社会带来持续和巨大的负担,但是临床指南和建议通常针对单一的精神疾病,而不是考虑多种精神疾病的综合管理[6]。目前对精神健康共病现象发生的机制知之甚少[7]。笔者通过综述儿童青少年精神疾病为核心的共病流行与病因机制,并对儿童青少年此类共病问题的未来研究方向进行探讨。
1. 儿童青少年精神健康为核心的共病负担
1.1 儿童青少年精神健康为核心的共病负担不容乐观
美国耶鲁大学Feinstein教授于1970年首次提出“共病”的概念,即同一患者在符合一种疾病诊断标准的同时,还符合其他疾病的诊断标准[8]。随着研究的发展,共病的概念逐渐外延,本研究中精神健康为核心的共病问题表现为多种健康问题的共发和共存。以往研究更多地关注共病负担较重的老年人,而忽略了儿童青少年人群,但事实上精神障碍病例中有一半在14岁前发展[9]。与此同时,儿童青少年时期的健康问题对整个生命周期具有重要的影响,有研究发现共病率随年龄增长而增加,且共病积累呈非线性,随着年龄的增长而加速[10]。尤其是在精神健康方面,一项针对27个国家的41项研究元分析结果显示,儿童青少年精神障碍的全球总患病率为13.4%[11]。有研究对来自8个国家18 282名儿童的流行病学数据进行的元分析结果显示,儿童各类精神健康问题共发的检出率为6.4%[12]。一项43 283名3~17岁美国儿童的精神健康调查结果显示,在罹患抑郁障碍的儿童青少年中,近3/4报告同时存在焦虑障碍[13]。
1.2 儿童青少年精神健康为核心的共病表现
1.2.1 儿童青少年常见的精神行为问题共病
焦虑和抑郁是儿童青少年发病率最高的两种精神疾病,多项临床研究显示二者共病现象较为常见[14-16]。一般来说,女生的焦虑和抑郁共病率高于男生,青春期时尤为明显[17]。Brady等[18]的1992年研究提出青少年的焦虑和抑郁之间存在着有意义的联系;此后学界对青少年焦虑抑郁共病的研究呈指数增长[15]。英国一项研究评估286名大学生的焦虑、抑郁症状,结果发现大学生焦虑和抑郁症状的共病率为27.8%[19]。一项中国江苏省大学生的调查结果显示,在新冠病毒感染疫情期间,处于极度紧张状态的学生更容易出现焦虑和抑郁症状[20]。在青少年抑郁症患者中,焦虑症是最常见的共病性精神健康障碍,共病率估计在15%~75%[14]。共病性焦虑抑郁与单一类型不同,如与非焦虑型重度抑郁症患者相比,焦虑型重度抑郁症患者有更严重的损伤和更多的自杀意念[21]。
注意缺陷多动障碍(attention-deficit/hyperactivity disorder, ADHD)与其他精神问题共病是另一类常见共病,单纯针对一类症状的治疗并不能完全缓解其全部症状。如ADHD与孤独症谱系障碍(autism spectrum disorder, ASD)两者可能存在共同的致病因素,在ASD患儿中常有注意缺陷、多动、冲动的症状;ADHD患儿中,社会交往障碍、语言障碍甚至刻板行为出现的频率较正常人群更高[22-23]。在病因分析上,一项全基因组关联研究表明,ADHD与其他精神疾病具有相同的因果位点[24]。一项关于增强神经成像遗传学的元分析研究发现,各类精神疾病中结构性磁共振成像表型具有实质性的相似性,且这些相似性在一定程度上可以通过共同遗传变异结构的相应相似性解释[25]。
1.2.2 儿童青少年精神行为问题同型和异型共发
儿童青少年的生长发育不平衡会导致躯体疾病或躯体-心理问题聚集[26]。儿童时期所存在的精神行为问题一般不会独立存在[15],精神健康问题在个体内部表现出强烈的集中趋势,即使是在外化和内化问题等看似不同的领域[27]。当问题行为属于同一诊断组,即个体内的多重内化或多重外化问题行为同时发生,即为同型共发[28]。儿童青少年中最常见的同型共发包括焦虑和抑郁的共发、对立违抗性障碍(oppositional defiant disorder,ODD)和品行障碍(conduct disorder,CD)的共发、ADHD和ODD /CD的共发。异型共发是指不同诊断组的问题行为同时发生,即个体的内化症状和外化症状同时发生[28]。儿童青少年最常见的异型共发为焦虑和ADHD的共发、抑郁和CD的共发、焦虑和ODD的共发。在临床上,儿童ADHD与其他精神症状(如焦虑、抽动、易怒、抑郁情绪、行为问题和药物使用)共同存在的现象很常见[29]。其中焦虑障碍是ADHD患者最常见的共病之一,有流行病学和临床研究表明,儿童青少年和成人的ADHD和焦虑障碍共病率很高[30]。
1.2.3 儿童青少年身心问题共病
儿童青少年精神健康问题和生理问题也存在多种共病形式,尤其是各类炎症疾病中伴随的抑郁和焦虑症状。研究显示,在炎症性肠病患者中观察到抑郁症和焦虑症的患病率增加[31-32]。这种共病可能是脑-肠轴的激活导致的,即自主神经系统介导的儿茶酚胺释放和下丘脑-垂体-肾上腺轴(hypothalamic-pituitary-adrenal, HPA轴)的应激激素分泌,以及胃肠道对这种激活的反应,可能会在精神问题和肠道问题的共病中起作用[33]。研究也显示,心理治疗可能对炎症性肠病患者的疾病活动、焦虑、抑郁等问题产生有益影响[34]。
此外,肥胖儿童会表现出更多的心理健康问题,包括抑郁和焦虑等[35-37]。如有研究通过荟萃分析发现,肥胖患病率的增加将导致心理困扰增加0.6百分点[38]。最近的证据表明,肥胖可能导致下丘脑炎症,炎症可能影响下丘脑与认知和情绪重要区域的相互联系,同时可能导致HPA轴失调并影响单胺能系[39]。儿童青少年近视与抑郁、焦虑等心理问题也存在关联,如36项研究的元分析结果显示视力受损儿童的抑郁和焦虑得分均高于对照组,尤其是近视儿童;斜视手术可改善抑郁和焦虑症状[40]。
2. 儿童青少年精神健康为核心的共病机制研究
2.1 共病机制的4种主要假设
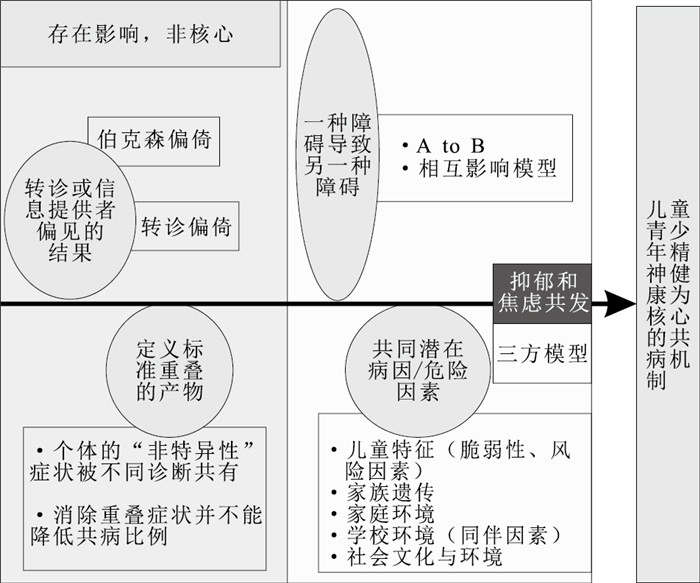
目前存在4个主要的假设可解释高比例的精神健康共病问题。第一,共病可能是转诊或信息提供者偏见的结果。过去共病研究通常基于临床样本,结果很可能受到转诊偏倚的影响,导致临床人群的共病率高于普通人群[41]。第二,共病可能是定义标准重叠的产物。研究指出,焦虑和抑郁的共病可能是心理疾病诊断系统的结果[18],即共病可能是由于个体的“非特异性”症状被不同的诊断共有,结果在诊断系统中造成了一定数量的疾病重叠[41],实际上这些疾病并不存在高于偶然水平的共发情况。但后续有研究并不支持该假设,通过在341名临床转诊儿童中控制重叠症状后重新评估诊断,研究者发现消除重叠症状并不能降低共病比例[42]。这支持共病是一种真实的现象,而不是方法学或定义上的缺陷。第三,一种障碍可能通过影响个体的发展轨迹而导致另一种障碍。以抑郁和越轨行为为例,这两种疾病之间可能存在3种关联,一种观点认为抑郁症状先于并预示着后期的越轨行为,有部分研究为这一假设提供了支持[43];同时也有一些证据表明越轨行为先于抑郁症状,如Giessena等[44]观察到13和14岁时的越轨行为与1年后的抑郁症状之间存在正相关;第三种视角被称为相互影响模型,认为抑郁症状和越轨行为存在双向关系,这一观点也得到了许多研究者的支持[45-46]。第四,两种疾病之间的共病可能有共同的潜在病因或危险因素[47]。一方面,一种疾病的风险因素可能与另一种疾病的风险因素相同;另一方面,尽管两种疾病的危险因素不同,但这些危险因素可能相互关联。儿童青少年精神问题共病的共同风险因素包括青少年特征的脆弱性、家族(遗传)传播以及家庭和家庭外环境等[48]。有研究发现,父母精神病理、情绪调节和认知偏见等风险因素可能是抑郁和越轨行为共同发生的基础[49]。也有研究通过21项纵向队列的4 337对母子数据分析发现,母亲童年时期的虐待经历是其后代疾病易感性的风险因素,且母亲暴露于多种形式的虐待与其后代健康结果的风险增加相关,即存在剂量-反应关系[50]。有学者通过澳大利亚两个儿童队列的研究发现,孕妇在怀孕期间吸烟均与儿童时期更多的外化症状如多动相关[51]。目前在精神健康共病研究中应用更多的是后两种假设,如图 1所示。
2.2 焦虑抑郁共病的病因学模型
目前解释焦虑和抑郁共病的模型主要是三方模型[52],该模型认为焦虑和抑郁有一个共同负面情感(negative affect, NA)因素,同时可分别通过生理过度觉醒(physiological hyperarousal,PH)和快感缺乏(positive affect, PA)两个特殊因素来区分,共同的NA因素能够解释焦虑和抑郁之间的共病[52]。大量的研究进一步证实了抑郁和焦虑共病的三方模型[53-54],如有研究通过对891名俄勒冈州患有抑郁症的青少年的4次纵向诊断数据的分析和比较,发现三方模型比单因素模型更能拟合数据[54]。但也有元分析结果显示,三方模型对于成人的抑郁和焦虑共病原因解释力较强,还需要对儿童和青少年进行更多的研究[55-56]。
3. 儿童青少年精神健康为核心的共病研究展望
首先,儿童期精神疾病的发展是复杂的,对人群症状发展的平均估计可能会模糊具有不同症状发展模式的亚组[57]。外化症状和内化症状代表常见儿童精神疾病的两大领域,并且已有多项研究探索了症状发展的异质性,这些研究侧重于根据症状发展的差异确定发育类型,从而揭示了有关症状发展的病因、纵向风险、机制和后果等。如Wiggins等[58]通过美国家庭调查数据也区分了3个内化症状和外化行为问题症状的联合轨迹。有研究基于群体的多轨迹模型评估了1 620名7~15岁儿童青少年常见精神健康问题的综合发展轨迹,结果表明共发的精神健康问题的发展轨迹可以有效地总结为几类亚型[48]。儿童青少年精神健康问题共病的发育亚型是未来研究的方向。
其次,心理病理学网络认为精神障碍的出现与发展是症状在网络中激活扩散的过程[59],为理解精神障碍提供了全新的视角。该方法能够关注到不同精神疾病中局部症状的相互作用,并确定症状在网络中的重要性[60],以此确定中心症状来解释共病。有研究者通过4 405名儿童的纵向队列对8种精神障碍利用网络方法进行分析,结果发现局部症状可以构成症状集群,并且随着时间的推移保持稳定,其中最一致的是抑郁症和ODD之间的相互作用[61]。启示症状/障碍水平复杂网络的相互作用和相互影响是儿童期/青春期内在化和外在化精神病理之间联系的合理机制。
最后,未来研究可以考虑多维度干预精神健康的共病。根据生态系统理论,个体的发展受到微观、中观和宏观生态系统的影响,微观系统涉及个体本身,中观系统涉及与个人直接相关的,如家庭、社区、同伴、学校等,宏观系统通常包括政策、文化、社会规范等[62]。儿童青少年的体育运动有助于改善体重、心血管和肌肉健康以及减少抑郁和焦虑症状[63]。有研究表明,医疗保健干预例如自我管理、教育宣传等对多病患者自评的焦虑、抑郁和自我效能感有显著的正向影响[64]。目前针对儿童青少年精神健康为核心的共病问题多维干预研究相对较少,针对儿童青少年精神健康为核心共病问题的共同风险因素进行多维干预是未来研究可以考虑的方向。
-
[1] ALLEGRANTE J P, WELLS M T, PETERSON J C. Interventions to support behavioral self-management of chronic diseases[J]. Ann Rev Public Health, 2019, 40: 127-146. doi: 10.1146/annurev-publhealth-040218-044008 [2] NG C Y, THOMAS-URIBE M, YANG Y A, et al. Theory-based health behavior interventions for pediatric chronic disease management: a systematic review[J]. JAMA Pediatr, 2018, 172(12): 1177-1186. doi: 10.1001/jamapediatrics.2018.3039 [3] BARR P B, BIGDELI T B, MEYERS J L. Prevalence, comorbidity, and sociodemographic correlates of psychiatric disorders reported in the all of US research program[J]. JAMA Psychiat, 2022, 79(6): 622-628. doi: 10.1001/jamapsychiatry.2022.0685 [4] MORALES-MUÑOZ I, MALLIKARJUN P K, CHANDAN J S, et al. Impact of anxiety and depression across childhood and adolescence on adverse outcomes in young adulthood: a UK birth cohort study[J]. Br J Psychiatry, 2023, 222(5): 212-220. doi: 10.1192/bjp.2023.23 [5] LUO X, ZHOU Y, ZHENG R, et al. Association of health-risk behaviors and depressive symptoms and anxiety symptoms: a school-based sample of Chinese adolescents[J]. J Public Health (Oxf), 2020, 42(3): e189-e198. doi: 10.1093/pubmed/fdz115 [6] ROSBACH M, ANDERSEN J S. Patient-experienced burden of treatment in patients with multimorbidity: a systematic review of qualitative data[J]. PLoS One, 2017, 12(6): e0179916. doi: 10.1371/journal.pone.0179916 [7] CRESPO P A, NUNES B P, BARROS F C, et al. Multimorbidity and simultaneity of health risk factors, from adolescence to early adulthood: 1993 Pelotas Birth Cohort[J]. Prev Med, 2022, 155: 106932. doi: 10.1016/j.ypmed.2021.106932 [8] FEINSTEIN A R. The pre-therapeutic classification of co-morbidity in chronic disease[J]. J Chronic Dis, 1970, 23(7): 455-468. doi: 10.1016/0021-9681(70)90054-8 [9] PATEL V, FLISHER A J, Hetrick S, et al. Mental health of young people: a global public-health challenge[J]. Lancet, 2007, 369(9569): 1302-1313. doi: 10.1016/S0140-6736(07)60368-7 [10] KHANOLKAR A R, CHATURVEDI N, KUAN V, et al. Socioeconomic inequalities in prevalence and development of multimorbidity across adulthood: a longitudinal analysis of the MRC 1946 National Survey of Health and Development in the UK[J]. PLoS Med, 2021, 18(9): e1003775. doi: 10.1371/journal.pmed.1003775 [11] POLANCZYK G V, SALUM G A, SUGAYA L S, et al. Annual research review: a Meta-analysis of the worldwide prevalence of mental disorders in children and adolescents[J]. J Child Psychol Psychiatry, 2015, 56(3): 345-365. doi: 10.1111/jcpp.12381 [12] VASILEVA M, GRAF R K, REINELT T, et al. Research review: a Meta-analysis of the international prevalence and comorbidity of mental disorders in children between 1 and 7 years[J]. J Child Psychol Psychiatry, 2021, 62(4): 372-381. doi: 10.1111/jcpp.13261 [13] GHANDOUR R M, SHERMAN L J, VLADUTIU C J, et al. Prevalence and treatment of depression, anxiety, and conduct problems in US children[J]. J Pediatr, 2019, 206: 256-267. doi: 10.1016/j.jpeds.2018.09.021 [14] CUMMINGS C M, CAPORINO N E, KENDALL P C. Comorbidity of anxiety and depression in children and adolescents: 20 years after[J]. Psychol Bull, 2014, 140(3): 816-845. doi: 10.1037/a0034733 [15] JENKINS J H, SANCHEZ G, MILLER E A, et al. Depression and anxiety among multiethnic middle school students: age, gender, and sociocultural environment[J]. Int J Soc Psychiatry, 2023, 69(3): 784-794. doi: 10.1177/00207640221140282 [16] CASTELPIETRA G, KNUDSEN A K S, AGARDH E E, et al. The burden of mental disorders, substance use disorders and self-harm among young people in Europe, 1990-2019: findings from the global burden of disease study[J]. Lancet Reg Health Eur, 2022, 16: 100341. doi: 10.1016/j.lanepe.2022.100341 [17] LONG E E, YOUNG J F, HANKIN B L. Separating within-person from between-person effects in the longitudinal co-occurrence of depression and different anxiety syndromes in youth[J]. J Res Person, 2019, 81: 158-167. doi: 10.1016/j.jrp.2019.06.002 [18] BRADY E U, KENDALL P C. Comorbidity of anxiety and depression in children and adolescents[J]. Psychol Bull, 1992, 111(2): 244-255. doi: 10.1037/0033-2909.111.2.244 [19] JENKINS P E, DUCKER I, GOODING R, et al. Anxiety and depression in a sample of UK college students: a study of prevalence, comorbidity, and quality of life[J]. J Am Coll Health, 2021, 69(8): 813-819. doi: 10.1080/07448481.2019.1709474 [20] QIN B, HU Z, LIU W, et al. Anxiety and depression among college students during the COVID-19 lockdown: a cross-sectional survey in Jiangsu, China[J]. Risk Manag Healthc Policy, 2023, 16: 711-723. doi: 10.2147/RMHP.S404478 [21] FAVA M, ALPERT J E, CARMIN C N, et al. Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D[J]. Psychol Med, 2004, 34(7): 1299-1308. doi: 10.1017/S0033291704002612 [22] DI MARTINO A, ZUO X N, KELLY C, et al. Shared and distinct intrinsic functional network centrality in autism and attention-deficit/hyperactivity disorder[J]. Biol Psychiatry, 2013, 74(8): 623-632. doi: 10.1016/j.biopsych.2013.02.011 [23] MORRIS S M, ACOSTA M T, GARG S, et al. Disease burden and symptom structure of autism in neurofibromatosis type 1: a study of the international NF1-ASD consortium team (INFACT)[J]. JAMA Psychiat, 2016, 73(12): 1276-1284. doi: 10.1001/jamapsychiatry.2016.2600 [24] SMOLLER J W, ANDREASSEN O A, EDENBERG H J, et al. Psychiatric genetics and the structure of psychopathology[J]. Mol Psychiatry, 2019, 24(3): 409-420. doi: 10.1038/s41380-017-0010-4 [25] RADONJIC N V, HESS J L, ROVIRA P, et al. Structural brain imaging studies offer clues about the effects of the shared genetic etiology among neuropsychiatric disorders[J]. Mol Psychiatry, 2021, 26(6): 2101-2110. doi: 10.1038/s41380-020-01002-z [26] 宋逸, 马军. 纠正生长发育不平衡预防儿童青少年重要共病[J]. 中华预防医学杂志, 2023, 57(4): 451-456.SONG Y, MA J. Correct the imbalance of growth and development and prevent important comorbidities of children and adolescents[J]. Chin J Prev Med, 2023, 57(4): 451-456. (in Chinese) [27] BEAUCHAINE T P, CICCHETTI D. A new generation of comorbidity research in the era of neuroscience and research domain criteria[J]. Dev Psychopathol, 2016, 28(4pt1): 891-894. doi: 10.1017/S0954579416000602 [28] MCDONOUGH-CAPLAN H, KLEIN D N, BEAUCHAINE T P. Comorbidity and continuity of depression and conduct problems from elementary school to adolescence[J]. J Abnorm Psychol, 2018, 127(3): 326-337. doi: 10.1037/abn0000339 [29] MORDRE M, GROHOLT B, KJELSBERG E, et al. The impact of ADHD and conduct disorder in childhood on adult delinquency: a 30 years follow-up study using official crime records[J]. BMC Psychiatry, 2011, 11: 57. doi: 10.1186/1471-244X-11-57 [30] KOYUNCU A, AYAN T, INCE GULIYEV E, et al. ADHD and anxiety disorder comorbidity in children and adults: diagnostic and therapeutic challenges[J]. Curr Psychiatry Rep, 2022, 24(2): 129-140. doi: 10.1007/s11920-022-01324-5 [31] HUARCAYA-VICTORIA J, BARRETO J, AIRE L, et al. Mental health in COVID-2019 survivors from a general hospital in Peru: sociodemographic, clinical, and inflammatory variable associations[J]. Int J Ment Health Addict, 2023, 21(2): 1264-1285. doi: 10.1007/s11469-021-00659-z [32] JONATHAN B, SONIA S, IRENE P, et al. Depression in individuals who subsequently develop inflammatory bowel disease: a population-based nested case-control study[J]. Gut, 2021, 70(9): 1642. doi: 10.1136/gutjnl-2020-322308 [33] MARGOLIS K G, CRYAN J F, MAYER E A. The microbiota-gut-brain axis: from motility to mood[J]. Gastroenterology, 2021, 160(5): 1486-1501. doi: 10.1053/j.gastro.2020.10.066 [34] 赵媛媛, 张媛媛, 吴振云, 等. 认知行为干预对炎症性肠病患者焦虑、抑郁及生活质量影响的Meta分析[J]. 中华现代护理杂志, 2018, 24(19): 2297-2302. doi: 10.3760/cma.j.issn.1674-2907.2018.19.016ZHAO Y Y, ZHANG Y Y, WU Z Y, et al. Effects of cognitive-behavioral intervention on anxiety, depression and life quality in inflammatory bowel disease patients: a Meta analysis[J]. Chin J Modern Nurs, 2018, 24(19): 2297-2302. (in Chinese) doi: 10.3760/cma.j.issn.1674-2907.2018.19.016 [35] STUBBS M A, CLARK V L, GIBSON P G, et al. Associations of symptoms of anxiety and depression with health-status, asthma control, dyspnoea, dysfunction breathing and obesity in people with severe asthma[J]. Respir Res, 2022, 23(1): 341. doi: 10.1186/s12931-022-02266-5 [36] PLACKETT B. The vicious cycle of depression and obesity[J]. Nature, 2022, 608(7924): S42-S43. doi: 10.1038/d41586-022-02207-8 [37] SMITH J D, FU E, KOBAYASHI M A. Prevention and management of childhood obesity and its psychological and health comorbidities[J]. Annu Rev Clin Psychol, 2020, 16: 351-378. doi: 10.1146/annurev-clinpsy-100219-060201 [38] JOKELA M, LAAKASUO M. Obesity as a causal risk factor for depression: systematic review and Meta-analysis of Mendelian Randomization studies and implications for population mental health[J]. J Psychiatr Res, 2023, 163: 86-92. doi: 10.1016/j.jpsychires.2023.05.034 [39] DIONYSOPOULOU S, CHARMANDARI E, BARGIOTA A, et al. The role of hypothalamic inflammation in diet-induced obesity and its association with cognitive and mood disorders[J]. Nutrients, 2021, 13(2): 498. doi: 10.3390/nu13020498 [40] LI D, CHAN V F, VIRGILI G, et al. Impact of vision impairment and ocular morbidity and their treatment on depression and anxiety in children: a systematic review[J]. Ophthalmology, 2022, 129(10): 1152-1170. doi: 10.1016/j.ophtha.2022.05.020 [41] ANGOLD A, COSTELLO E J, ERKANLI A. Comorbidity[J]. J Child Psychol Psychiatry, 1999, 40(1): 57-87. doi: 10.1111/1469-7610.00424 [42] BIEDERMAN J, FARAONE S, MICK E, et al. Psychiatric comorbidity among referred juveniles with major depression: fact or artifact?[J]. J Am Acad Child Adolesc Psychiatry, 1995, 34(5): 579-590. doi: 10.1097/00004583-199505000-00010 [43] KOFLER M J, MCCART M R, ZAJAC K, et al. Depression and delinquency covariation in an accelerated longitudinal sample of adolescents[J]. J Consult Clin Psychol, 2011, 79(4): 458-469. doi: 10.1037/a0024108 [44] GIESSENA V D, BRANJEA S J T, OVERBEEKA G, et al. Co-occurrence of aggressive behavior and depressive symptoms in early adolescence: a longitudinal multi-informant study[J]. Eur Rev Appl Psychol, 2013, 63(4), 193-201. doi: 10.1016/j.erap.2013.03.001 [45] CHEN C Y, LIEN Y J. Trajectories of co-occurrence of depressive symptoms and deviant behaviors: the influences of perceived social support and personal characteristics[J]. Child Youth Serv Rev, 2018, 95: 174-182. doi: 10.1016/j.childyouth.2018.10.037 [46] NOCENTINI A, CALAMAI G, MENESINI E. Codevelopment of delinquent and depressive symptoms across adolescence: time-invariant and time-varying effects of school and social failure[J]. J Clin Child Adolesc Psychol, 2012, 41(6): 746-759. doi: 10.1080/15374416.2012.728155 [47] CAPALDI D M, STOOLMILLER M. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: Ⅲ. Prediction to young-adult adjustment[J]. Dev Psychopathol, 1999, 11(1): 59-84. doi: 10.1017/S0954579499001959 [48] MURRAY A L, EISNER M, NAGIN D, et al. A multi-trajectory analysis of commonly co-occurring mental health issues across childhood and adolescence[J]. Eur Child Adolesc Psychiatry, 2022, 31(1): 145-159. doi: 10.1007/s00787-020-01679-1 [49] WOLFF J C, OLLENDICK T H. The comorbidity of conduct problems and depression in childhood and adolescence[J]. Clin Child Fam Psychol Rev, 2006, 9(3-4): 201-220. doi: 10.1007/s10567-006-0011-3 [50] MOOG N K, CUMMINGS P D, JACKSON K L, et al. Intergenerational transmission of the effects of maternal exposure to childhood maltreatment in the USA: a retrospective cohort study[J]. Lancet Public Health, 2023, 8(3): e226-e237. doi: 10.1016/S2468-2667(23)00025-7 [51] FREATHY R M, MOOK-KANAMORI D O, SOVIO U, et al. Variants in ADCY5 and near CCNL1 are associated with fetal growth and birth weight[J]. Nat Genet, 2010, 42(5): 430-435. doi: 10.1038/ng.567 [52] CLARK L A, WATSON D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications[J]. J Abnorm Psychol, 1991, 100(3): 316-336. doi: 10.1037/0021-843X.100.3.316 [53] TULLY P J, ZAJAC I T, VENNING A J. The structure of anxiety and depression in a normative sample of younger and older Australian adolescents[J]. J Abnorm Child Psychol, 2009, 37(5): 717-726. doi: 10.1007/s10802-009-9306-4 [54] OLINO T M, KLEIN D N, LEWINSOHN P M, et al. Longitudinal associations between depressive and anxiety disorders: a comparison of two trait models[J]. Psychol Med, 2008, 38(3): 353-363. doi: 10.1017/S0033291707001341 [55] ANDERSON E R, HOPE D A. A review of the tripartite model for understanding the link between anxiety and depression in youth[J]. Clin Psychol Rev, 2008, 28(2): 275-287. doi: 10.1016/j.cpr.2007.05.004 [56] 耿梦龙, 陶芳标. 儿童内外化行为共病现象及对未来发展的影响[J]. 中国学校卫生, 2018, 39(4): 637-640. doi: 10.16835/j.cnki.1000-9817.2018.04.048GENG M L, TAO F B. Comorbidities of children's internalizing and externalizing behaviors and their influence on future development[J]. Chin J Sch Health, 2018, 39(4): 637-640. (in Chinese) doi: 10.16835/j.cnki.1000-9817.2018.04.048 [57] PATALAY P, FINK E, FONAGY P, et al. Unpacking the associations between heterogeneous externalising symptom development and academic attainment in middle childhood[J]. Eur Child Adolesc Psychiatry, 2016, 25(5): 493-500. doi: 10.1007/s00787-015-0758-5 [58] WIGGINS J L, MITCHELL C, HYDE L W, et al. Identifying early pathways of risk and resilience: the codevelopment of internalizing and externalizing symptoms and the role of harsh parenting[J]. Dev Psychopathol, 2015, 27(4 Pt 1): 1295-1312. [59] EPSKAMP S, BORSBOOM D, FRIED E I. Estimating psychological networks and their accuracy: a tutorial paper[J]. Behav Res Methods, 2018, 50(1): 195-212. doi: 10.3758/s13428-017-0862-1 [60] CAI H, ZHAO Y J, HE F, et al. Internet addiction and residual depressive symptoms among clinically stable adolescents with major psychiatric disorders during the COVID-19 pandemic: a network analysis perspective[J]. Transl Psychiatry, 2023, 13(1): 186. doi: 10.1038/s41398-023-02468-5 [61] MCELROY E, SHEVLIN M, MURPHY J, et al. Co-occurring internalizing and externalizing psychopathology in childhood and adolescence: a network approach[J]. Eur Child Adolesc Psychiatry, 2018, 27(11): 1449-1457. doi: 10.1007/s00787-018-1128-x [62] Bronfenbrenner U. The ecology of human development[M]. Cambridge, MA: Harvard University Press, 1979. [63] POITRAS V J, GRAY C E, BORGHESE M M, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth[J]. Appl Physiol Nutr Metab, 2016, 41(6 Suppl 3): S197-239. [64] LEE H J, LEE M, HA J H, et al. Effects of healthcare interventions on psychosocial factors of patients with multimorbidity: a systematic review and Meta-analysis[J]. Arch Gerontol Geriatr, 2020, 91: 104241. doi: 10.1016/j.archger.2020.104241 期刊类型引用(6)
1. 戴彪,曹银,孙艳红,张元元,夏清荣. 808例抗精神病药品不良反应报告分析. 中国药物警戒. 2025(01): 99-103+108 .  百度学术
百度学术2. 董彬,冯天舒,宋逸. 以高质量学校卫生标准为牵引推动学生常见病多病共防. 中华预防医学杂志. 2025(02): 138-143 .  百度学术
百度学术3. 黄天彧,蔡珊,张依航,李佳欣,孙子曰,杨田,高建琼,董彦会,星一,张秀红,宋逸. 2019—2022年内蒙古自治区13~18岁青少年多病流行状况及其与中高强度身体活动的关联分析. 中华预防医学杂志. 2025(02): 189-194 .  百度学术
百度学术4. 娄芳,葛玉杰,赵晶,娄涛,张艳萍. 某三级甲等精神专科医院近3年青少年精神障碍疾病构成变化及其影响因素分析. 临床心身疾病杂志. 2024(02): 117-121 .  百度学术
百度学术5. 王超. 针对性健康教育在青少年精神障碍患儿父母中的应用. 妇儿健康导刊. 2024(23): 174-178 .  百度学术
百度学术6. 宋逸,张秀红,马军. 儿童青少年主要健康问题“共病-共因-共防”机制建立与探索. 中国学校卫生. 2023(09): 1281-1285 .  本站查看
本站查看其他类型引用(2)
-








 下载:
下载:
 下载:
下载:

