Childhood blood pressure trajectory and its association with overweight and obesity
-
摘要:
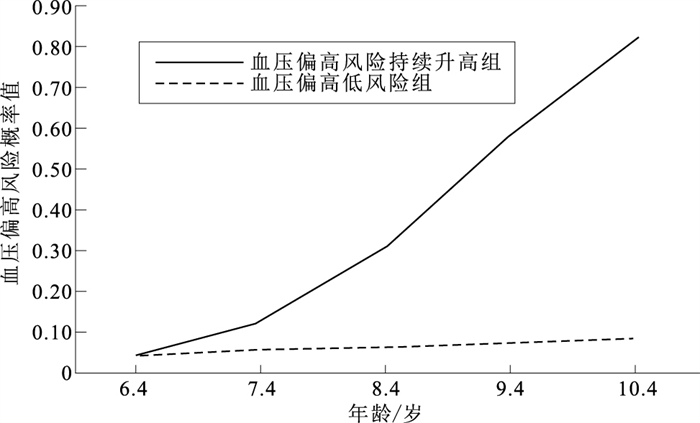
目的 分析儿童血压发育的轨迹及其与超重肥胖的关系,为儿童血压偏高的防控提供科学依据。 方法 利用“自贡基于学校的心血管代谢风险队列研究”,纳入1 177名接受5次血压测量的儿童,使用中国儿童血压参照标准判断儿童的血压状态。基于群组的轨迹模型探索儿童血压的发育轨迹,采用Logistic模型分析儿童血压发育轨迹与超重肥胖出现次数的关系。 结果 儿童5次测量血压偏高的流行率分别为1.9%,6.6%,7.0%,12.5%和11.2%。儿童血压的发育轨迹分为血压偏高的低风险组和血压偏高风险持续升高组。血压偏高的低风险组,其血压偏高的风险随着年龄的增长而较为平稳。血压偏高风险持续升高组,其血压偏高的风险随着年龄的增长而明显增加。Logistic回归分析显示,研究期间出现超重肥胖次数越多的儿童,其血压偏高风险升高(OR=1.34,95%CI=1.17~1.53,P < 0.01)。 结论 儿童血压的发育轨迹不同,超重肥胖儿童的血压偏高风险随着年龄的增长而明显增加。需关注超重肥胖儿童的血压发育轨迹,预防其出现血压偏高。 Abstract:Objective To analyze the childhood blood pressure (BP) trajectory and its relationship with overweight and obesity, to provide evidence regarding prevention and control of childhood elevated BP. Methods A total of 1 177 children who participated in five surveys of Zigong school-based cardiometabolic risks survey. Elevated BP was defined by using National BP reference for Chinese children. Group-based trajectory model was used to identify distinct BP trajectories. Logistic models were conducted to investigate the association of number of overweight/obesity across surveys with BP trajectory. Results In the five consecutive waves, the corresponding prevalence of elevated BP was 1.9%, 6.6%, 7.0%, 12.5% and 11.2%. Childhood BP trajectory were classified into constant low and high increasing risk of elevated BP groups. The risk of elevated BP increased at a steady rate with age in constant low risk of elevated BP groups, while the risk of elevated BP increased dramatically with age in high increasing risk of elevated BP groups. Logistic regression analysis showed that those with increasing number of occurrence of overweight/obesity tended to be classified into high increasing risk of elevated BP group(OR=1.34, 95%CI=1.17-1.53, P < 0.01). Conclusion Blood pressure trajectory during childhood varies. The risk of elevated BP increased dramatically with age in overweight and obese children. Attention should be paid to the BP trajectory of overweight and obese children to prevent elevated BP. -
Key words:
- Blood pressure /
- Overweight /
- Obesity /
- Regression analysis /
- Child
1) 利益冲突声明 所有作者声明无利益冲突。 -
表 1 研究期间出现超重肥胖的次数与血压发育轨迹的关系
Table 1. Association between number of overweight and obesity and blood pressure trajectory
出现超重肥胖次数 人数 OR值(OR值95%CI) P值 1 94 1.34(0.39~4.62) 0.65 2 53 0.67(0.09~5.16) 0.70 3 48 1.64(0.37~7.40) 0.52 4 63 3.87(1.46~10.26) 0.01 5 143 4.06(2.01~8.23) < 0.01 -
[1] 中共中央, 国务院. "健康中国2030"规划纲要[R/OL]. (2016-10-25)[2022-02-11]. http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm.Central Committee of Communist Party of China, State Council of the PRC. The "healthy China 2030" planning outline[R/OL]. (2016-10-25)[2022-02-11]. http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm. [2] 国务院. 中国儿童发展纲要(2021-2030年)[R/OL]. (2021-09-27)[2022-02-11]. http://www.nwccw.gov.cn/2021-09/27/content_295436.htm.State Council of the PRC. Program for development of Chinese children(2021-2030)[R/OL]. (2021-09-27)[2022-02-11]. http://www.nwccw.gov.cn/2021-09/27/content_295436.htm. [3] FAN H, ZHANG X. Alarming trends in severe obesity in Chinese children from 1991 to 2015[J]. Child Obes, 2020, 16(4): 244-249. doi: 10.1089/chi.2019.0171 [4] 马淑婧, 羊柳, 赵敏, 等. 1991-2015年中国儿童青少年血压水平及高血压检出率的变化趋势[J]. 中华流行病学杂志, 2020, 41(2): 178-183. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGZ202102031.htmMA S J, YANG L, ZHAO M, et al. Changing trends in the levels of blood pressure and prevalence of hypertension among Chinese children and adolescents from 1991 to 2015[J]. Chin J Epidemiol, 2020, 41(2): 178-183. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGZ202102031.htm [5] FAN H, HOU D, LIU J, et al. Performance of 4 definitions of childhood elevated blood pressure in predicting subclinical cardiovascular outcomes in adulthood[J]. J Clin Hyperten (Greenwich), 2018, 20(3): 508-514. doi: 10.1111/jch.13201 [6] SUVILA K, MCCABE E L, LEHTONEN A, et al. Early onset hypertension is associated with hypertensive end-organ damage already by midLife[J]. Hypertension, 2019. DOI: 10.1161/HYPERTENSIONAHA.119.13069. [7] National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents[J]. Pediatrics, 2004, 114(2 Suppl 4th report): 555-576. [8] DONG J, DONG H, YAN Y, et al. Prevalence of hypertension and hypertension phenotypes after three visits in Chinese urban children[J]. J Hyperten, 2021. DOI: 10.1097/HJH.0000000000002977. [9] LIU K, LI C, GONG H, et al. Prevalence and risk factors for hypertension in adolescents aged 12 to 17 years: a school-based study in China[J]. Hypertension, 2021, 78(5): 1577-1585. doi: 10.1161/HYPERTENSIONAHA.121.17300 [10] MENG L, LIANG Y, LIU J, et al. Prevalence and risk factors of hypertension based on repeated measurements in Chinese children and adolescents[J]. Blood Press, 2013, 22(1): 59-64. doi: 10.3109/08037051.2012.701790 [11] 范晖, 康利, 刘宇丹. 儿童期体重状态及其变化与血压偏高发生风险的关系[J]. 现代预防医学, 2021, 48(5): 819-823. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF202105014.htmFAN H, KANG L, LIU Y D. Childhood weight status, its change and risk of elevated blood pressure[J]. Mod Prev Med, 2021, 48(5): 819-823. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYF202105014.htm [12] 范晖, 闫银坤, 米杰. 中国3~17岁儿童性别、年龄别和身高别血压参照标准[J]. 中华高血压杂志, 2017, 25(5): 428-435. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGZ201705010.htmFAN H, YAN Y K, MI J. Updating blood pressure references for Chinese children aged 3-17 years[J]. Chin J Hyperten, 2017, 25(5): 428-435. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGZ201705010.htm [13] 国家卫生和计划生育委员会. 学龄儿童青少年超重与肥胖筛查: WS/T 586-2018[S/OL]. (2018-08-01)[2022-02-11]. http://www.nhc.gov.cn/ewebeditor/uploadfile/2018/03/20180329094554367.pdf.Health and Family Planning Commission of the PRC. Screening for overweight and obesity among school-aged children and adolescents: WS/T 586-2018[S/OL]. (2018-08-01)[2022-02-11]. http://www.nhc.gov.cn/ewebeditor/uploadfile/2018/03/20180329094554367.pdf. [14] JONES B L, NAGIN D S. Advances in group-based trajectory modeling and an SAS procedure for estimating them[J]. Sociol Meth Res, 2007, 35(4): 542-571. doi: 10.1177/0049124106292364 [15] WANG X, HU J, HUANG S, et al. Exploring overweight risk trajectories during childhood and their associations with elevated blood pressure at late adolescence: a retrospective cohort study[J]. Hypertension, 2022, 79(8): 1605-1613. doi: 10.1161/HYPERTENSIONAHA.121.18714 [16] SUN J, STEFFEN L M, MA C, et al. Definition of pediatric hypertension: are blood pressure measurements on three separate occasions necessary[J]. Hyperten Res, 2017, 40(5): 496-503. doi: 10.1038/hr.2016.179 [17] LEE J W, KIM N, PARK B, et al. Blood pressure trajectory modeling in childhood: birth-cohort study[J]. Clin Hyperten, 2020, 26: 2. doi: 10.1186/s40885-019-0133-9 [18] THEODORE R F, BROADBENT J, NAGIN D, et al. Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes[J]. Hypertension, 2015, 66(6): 1108-1115. doi: 10.1161/HYPERTENSIONAHA.115.05831 [19] BRADY T M. Obesity-related hypertension in children[J]. Front Pediatr, 2017, 5: 197. doi: 10.3389/fped.2017.00197 [20] SOROF J, DANIELS S. Obesity hypertension in children: a problem of epidemic proportions[J]. Hypertension, 2002, 40(4): 441-447. doi: 10.1161/01.HYP.0000032940.33466.12 -







 下载:
下载: