Cumulative Meta-analysis of the association between obesity and autism spectrum disorders in children and adolescents
-
摘要:
目的 对肥胖和孤独症谱系障碍(ASD)流行病学研究进行Meta分析,以探究儿童青少年孤独症谱系障碍和肥胖之间的关联,为改善ASD儿童青少年患者日常生活质量提供一定指导作用。 方法 系统检索PubMed、CNKI(2010年1月—2022年1月)中与肥胖、ASD相关的文献,采用Meta分析报告OR值。并对权重、体质量指数(BMI)获得方式、年龄等分类指标进行亚组分析。 结果 共筛选11篇文献纳入分析,总样本包括336 830名参与者,其中ASD患者58 187名,正常发育者278 643名。经Meta分析,与正常人相比,ASD儿童青少年有更高的肥胖发病风险(OR=1.80,95%CI=1.74~1.86)。根据BMI获得方式分组后,与正常人相比,BMI由客观测量、从病历中获得、父母报告获得的ASD患者有更高的肥胖发病风险,OR值(OR值95%CI)分别为1.43(1.04~1.96),5.23(4.44~6.16),2.57(1.79~3.69)。根据年龄分组后,与正常人相比,14~20岁ASD儿童青少年患者有更高的肥胖发病风险,OR值(OR值95%CI)=2.19(1.21~3.94)。 结论 相较于正常发育同龄人,ASD儿童青少年患者发生肥胖的风险更高。应在饮食、体力活动方面正确引导ASD患者,尤其是在青春期,避免其发生肥胖及肥胖引起的其他疾病。 Abstract:Objective This study conducts a Meta-analysis on the epidemiological studies of obesity and autism spectrum disorder (ASD) in order to explore the relationship between autism spectrum disorder and obesity in children and adolescents, and to provide some guidance for improving the quality of daily life of children and adolescents with ASD. Methods PubMed and CNKI (January, 2010-January, 2022) were systematically searched for literature related to autism spectrum disorders reported the or value by Meta-analysis, and compared the weight, BMI acquisition method. Results A total of 11 literatures were selected for analysis. The total sample included 336 830 participants, including 58 187 patients with ASD and 278 643 patients with normal development. Through Meta-analysis, children and adolescents with ASD had a higher risk of obesity than normal people (OR=1.80, 95%CI=1.74-1.86). when stratified by BMI acquisition, autistic patients with BMI obtained from objective measurement, medical records and parents' reports had a higher risk of obesity than normal people, and the OR value (95%CI) was 1.43(1.04-1.96), 5.23(4.44-6.16), 2.57(1.79-3.69). When stratified by age, children and adolescents with ASD aged 14 to 20 years had a higher risk of obesity than normal people. The OR value (95%CI) was 2.19(1.21-3.94). Conclusion Compared with healthy peers, children and adolescents with ASD have a higher risk of obesity. ASD patients need guidance in diet and physical activity, especially in adolescence, to prevent obesity or diseases caused by obesity. -
Key words:
- Autistic disorder /
- Obesity /
- Meta-analysis /
- Child /
- Adolescent
1) 利益冲突声明 所有作者声明无利益冲突。 -
孤独症谱系障碍(autism spectrum disorder,ASD)是以社交沟通和互动受损,以及重复兴趣、刻板行为为特征的神经发育障碍[1-2]。近年来,流行病学调查数据显示,全球范围内ASD患病率在1%~2%[3]。ASD患者通常被认为有更高肥胖的风险。肥胖的定义为相较于同年龄、同性别的正常人,高于95%的体质量指数(BMI)[4]。肥胖对ASD儿童青少年患者存在极大的负面影响,如会引起糖尿病、抑郁症[5]等疾病,增加父母等照顾者的负担[6]。在世界不同地区,已经有多项观察性研究证实了儿童青少年的ASD患病率和肥胖发生风险之间的关系[7-11],但这些研究的结果并不一致,孤独症和肥胖风险之间的关联程度及潜在的混杂因素在解释孤独症与肥胖之间关联中的作用也并不清楚。因此,本研究搜索和整理2010年1月—2022年1月同类型研究,提取研究对象年龄分布在2~20岁的文献,进行系统回顾和荟萃分析而成的累积Meta分析。更加客观地评估与正常发育的同龄人相比,ASD儿童青少年患者肥胖的患病率在何种程度显著提高,为进一步探讨孤独症儿童青少年患者肥胖病因提供理论基础,为改善ASD儿童青少年患者日常生活质量提供一定指导作用。
1. 资料来源与方法
1.1 文献检索
系统地检索PubMed和CNKI (2010年1月—2022年1月),使用与肥胖、孤独症谱系障碍相关的检索词,在CNKI中采用高级检索“孤独症”或“自闭症”或“孤独症谱系障碍”和“肥胖”。在PubMed中采用search“ASD” OR “autism spectrum disorder” OR “autistic disorder” OR “autism” OR “ Asperger syndrome” and “obesity” OR “obese” OR“BMI”。
1.2 文献纳入与排除标准
纳入标准:(1)研究类型为国内外关于孤独症谱系障碍患者与孤独症的观察性研究;(2)发表时间为2010年1月—2022年1月;(3)有ASD患者与肥胖发病例数。排除标准: (1)非中文或英文发表的文章;(2)仅以摘要方式发表的文章;(3)综述类文章;(4)非观察性研究;(5)非人群研究;(6) 研究对象年龄范围不在2~20岁。
1.3 文献质量评价
研究质量的评价采用纽卡斯尔-渥太华评分量表(Newcastle-Ottawa Scale),该量表从研究对象选择、组间可比性、结果测量三方面、8个项目对研究质量进行评价,满分为9分。
1.4 纳入研究数据提取
首先,对文章的标题与摘要进行初步地评估,在此步骤中要求相对广泛,以保留尽可能多的研究。其次,由研究人员从初步筛选的文章进行全文阅读,根据上述纳入与排除标准,对文献的研究设计、研究对象及研究结果进行评价、选择。当信息不足,联系文章作者以获取需要的信息,若没有得到需要的信息,排除该文章。如果同一研究不同样本多次发表暴露与结局的关联,则保留样本量最大的研究。
1.5 数据采集
将数据信息从符合标准的文献中按照标准化记录表提取。提取信息包括发表时间,第一作者姓名,研究对象所在国家,样本量、年龄范围的样本量信息、肥胖的OR值及其95%CI。
1.6 统计学方法
使用Stata 15.0软件进行统计分析。对文献进行异质性检验,若I2 < 50%表明异质性小,若I2>50%表明异质性大。异质性检验P < 0.05,表明各研究总体间差异有统计学意义,选择随机效应模型结果,否则选择固定效应模型结果。计算合并OR值及其95%CI,评价ASD与肥胖发病风险的关系。使用Begg检验评估是否存在发表偏倚,若P < 0.1,则认为存在发表偏倚。
2. 结果
2.1 文献筛选结果
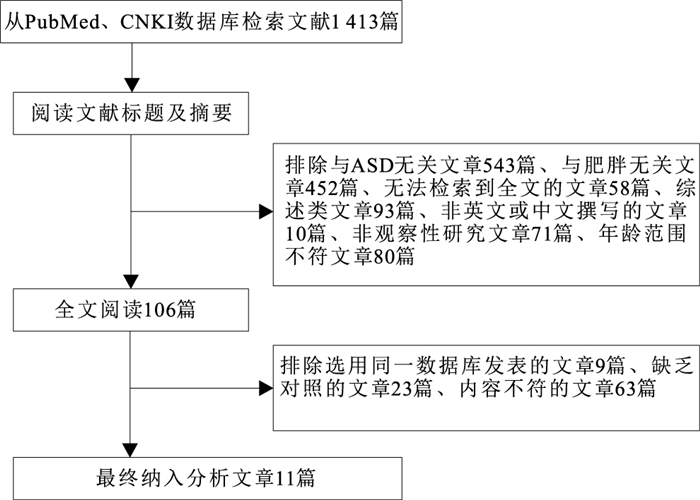
根据检索策略,从以上数据库共检索到文献1 413篇,筛查后最终纳入分析共11篇文献,见图 1。总样本包括336 830名参与者,其中ASD患者58 187名,正常发育者278 643名。使用纽卡斯尔-渥太华评分量表进行研究质量的评价,研究质量均较高,见表 1。
表 1 纳入文献的基本资料Table 1. Basic data included in the study第一作者与发表时间 国家 年龄/岁 ASD人数 正常发育人数 OR值(OR值95%CI) ASD诊断方法 BMI获得方式 纽卡斯尔-渥太华评估总分 Barnhill[12](2016) 美国 3~8 86 57 1.33(0.38~4.66) SCQ,ADI-R,ADOS 客观测量 6 Bicer[13](2016) 美国 6~8 118 97 1.77(1.02~3.09) DSM-IV,DSM-V 客观测量 8 Broder-Fingert[4](2014) 美国 2~20 2 976 3 696 5.23(4.44~6.16) ICD-9 从病历中获得 7 Castro[14](2016) 巴西 6~13 49 49 2.58(1.02~6.52) DSM-IV 客观测量 6 Hill[15](2015) 美国 2~17 5 053 8 844 1.10(1.00~1.20) DSM-IV,ADOS 客观测量 8 Kummer[16](2016) 巴西 4~12 69 19 5.00(0.62~40.56) DSM-V 客观测量 7 Liu[17](2016) 中国 3~7 154 73 0.42(0.19~0.91) DSM-V 客观测量 8 Phillips[18](2014) 美国 12~17 93 8 141 3.16(2.04~4.90) 父母报告 父母报告 6 Rimmer[19](2010) 美国 14~16 159 12 973 2.18(1.51~3.13) 父母报告 父母报告 6 Shedilock[20](2016) 美国 2~18 48 762 243 810 1.85(1.78~1.92) ICD-9-CM 客观测量 8 Levy[21](2019) 美国 2~5 668 884 1.57(1.24~2.00) ADOS,SCQ,ADI-R,DSM-V 客观测量 7 注:SCQ为社会沟通问卷,ADI-R为孤独症诊断访谈量表(修订版),ADOS为孤独症诊断观察时间表,DSM-IV为《诊断和统计手册》第4版,DSM-V为《诊断和统计手册》第5版,ICD-9为《国际疾病分类》第9版修订,ICD-9-CM为《国际疾病分类》第9版修订的临床修改。 2.2 确诊方法
11篇文献用于确定ASD的方法中,2项研究使用了父母报告,其他研究基于诊断的依据是《诊断和统计手册》(DSM-IV、DSM-V)、《社会沟通问卷》(SCQ)、《国际疾病分类》第9版修订(ICD-9)、《国际疾病分类》第9版的临床修订本(ICD-9-CM)、ADI-R、ADOS。对于确定BMI的方法,2项研究使用父母报告的数据,8项研究客观地测量了数据,1项研究从参与者的病历中提取了信息。见表 1。
2.3 孤独症与肥胖风险的Meta分析结果
异质性检验结果显示,I2>75%,P < 0.05,各项研究之间存在异质性,采用随机效应模型进行效应合并分析。结果显示,与正常人相比,孤独症患者有更高的肥胖发病的风险(OR=1.80,95%CI=1.74~1.86)。
文献[20]和[15]所占权重较大,为避免由这2篇文献主导的潜在的混杂因素,故去掉这2篇文章后再次采用随机效应模型进行效应合并分析,结果显示,I2=92.4%,与正常人相比,孤独症患者有更高的肥胖发病的风险(OR=3.07,95%CI=2.74~3.45)。
为排除BMI获取方式不同产生的偏倚,根据各文献所提供的获取BMI的方式将文献分组,按BMI获得方式将文献分为3类(客观测量[12-17, 20-21]、从病历中获得[4]、父母报告[18-19])做亚组分析。结果显示,与正常人相比,BMI由客观测量、从病历中获得、父母报告获得的孤独症患者有更高的肥胖发病风险,OR值(95%CI)分别为1.43(1.04~1.96),5.23(4.44~6.16),2.57(1.79~3.69)。
为解释样本年龄对肥胖风险产生的影响,按文献提供的研究对象的年龄将文献分为3组进行亚组分析。组别1中包含文献[12-14, 16-17, 21]的年龄分布在2~13岁,组别2中包含文献[18-19]的年龄分布在14~20岁,组别3中包含文献[4, 15, 20]的年龄分布在2~20岁。结果显示,与正常人相比,14~20岁ASD儿童青少年患者有更高的肥胖发病风险,OR值(95%CI)=2.19(1.21~3.94)。
2.4 发表偏倚评价
以效应量ln hr及其标准误为变量,对发表偏倚进行估计。经Begg test检验所得P=0.59,提示不存在明显的发表偏倚。
3. 讨论
本研究结果显示,与同龄正常发育者相比,ASD儿童青少年患者有更高的肥胖发病风险。肥胖已被认为是可引起2型糖尿病、心血管疾病等多种疾病的重要危险因素[22-23]。已有多项观察性研究对ASD与发生肥胖之间的关系进行探究,但是其潜在的关联机制尚无定论。在一般人群中,睡眠时间不足与儿童肥胖的风险之间存在明显的关联[24]。与正常发育的儿童相比,ASD儿童的睡眠时间和质量较差,并且不会随着年龄的增长而改善[25]。与正常的同龄人相比,患有ASD的儿童青少年通常饮食习惯异常,会食用更多的高能量食品,但水果和蔬菜摄入较少[26]。并且患有ASD的儿童青少年常常会有挑食行为,可能与食物的质地、颜色、气味有关。食物的选择与接受与否相关,并与肥胖有关联[27]。
经亚组分析发现,患ASD的青少年有更高的肥胖发病风险。在能量消耗方面,随着ASD儿童年龄的增长,其参与体育活动的机会可能会减少。相较于ASD儿童,患有ASD的年龄较大的青少年通常更专注于电子产品,这可能是其限制性兴趣、社交障碍的表现。并且运动和社交技能以及沟通困难会导致其久坐不动[27]。随着ASD儿童年龄的增长和体型的增大,父母可能更难以约束使其进行体育活动,也更难阻止儿童进行久坐行为[28]。
本研究针对ASD儿童青少年患者与肥胖发生风险关系的观察性研究进行Meta分析有以下优势:(1)对之前所做的Meta分析的数据进行更新;(2)根据各文献所提供的获取BMI的方式将文献分组,排除了因BMI获取方式不同产生的系统误差;(3)按文献提供的研究对象的年龄分组,进行亚组分析,解释样本年龄对肥胖风险产生的影响,在青春期ASD患者更易发生肥胖问题,这与青春期的生长发育特点、ASD患者自身的生活习惯、体力活动等密切相关;(4)通过Begg检验对发表偏倚进行了评价,结果显示不存在明显的发表偏倚,结果较为可靠。
本研究也存在一定的局限性,对于Meta分析而言,已发表与未发表的研究可能存在系统差异,研究结果为阳性的文章较容易发表,可能容易得到有统计学意义的结果,产生发表偏倚,影响结果的真实性。由于本研究检索了英文和中文文献,在筛选后仅选出英文文献,因此,语种的选择偏倚可能对结果会造成一定影响。
未来的相关研究可以聚焦于讨论ASD儿童青少年患者肥胖风险高于正常人的原因,如个人饮食习惯、进餐仪式感、体育活动参与情况、视屏时间等。此外,未来针对ASD儿童青少年患者共患肥胖情况,也应予以充分重视,探究出更合理的改善措施。
-
表 1 纳入文献的基本资料
Table 1. Basic data included in the study
第一作者与发表时间 国家 年龄/岁 ASD人数 正常发育人数 OR值(OR值95%CI) ASD诊断方法 BMI获得方式 纽卡斯尔-渥太华评估总分 Barnhill[12](2016) 美国 3~8 86 57 1.33(0.38~4.66) SCQ,ADI-R,ADOS 客观测量 6 Bicer[13](2016) 美国 6~8 118 97 1.77(1.02~3.09) DSM-IV,DSM-V 客观测量 8 Broder-Fingert[4](2014) 美国 2~20 2 976 3 696 5.23(4.44~6.16) ICD-9 从病历中获得 7 Castro[14](2016) 巴西 6~13 49 49 2.58(1.02~6.52) DSM-IV 客观测量 6 Hill[15](2015) 美国 2~17 5 053 8 844 1.10(1.00~1.20) DSM-IV,ADOS 客观测量 8 Kummer[16](2016) 巴西 4~12 69 19 5.00(0.62~40.56) DSM-V 客观测量 7 Liu[17](2016) 中国 3~7 154 73 0.42(0.19~0.91) DSM-V 客观测量 8 Phillips[18](2014) 美国 12~17 93 8 141 3.16(2.04~4.90) 父母报告 父母报告 6 Rimmer[19](2010) 美国 14~16 159 12 973 2.18(1.51~3.13) 父母报告 父母报告 6 Shedilock[20](2016) 美国 2~18 48 762 243 810 1.85(1.78~1.92) ICD-9-CM 客观测量 8 Levy[21](2019) 美国 2~5 668 884 1.57(1.24~2.00) ADOS,SCQ,ADI-R,DSM-V 客观测量 7 注:SCQ为社会沟通问卷,ADI-R为孤独症诊断访谈量表(修订版),ADOS为孤独症诊断观察时间表,DSM-IV为《诊断和统计手册》第4版,DSM-V为《诊断和统计手册》第5版,ICD-9为《国际疾病分类》第9版修订,ICD-9-CM为《国际疾病分类》第9版修订的临床修改。 -
[1] MORRIS-ROSENDAHL D J, CROCQ M A. Neurodevelopmental disorders-the history and future of a diagnostic concept[J]. Dialogues Clin Neurosci, 2020, 22(1): 65-72. doi: 10.31887/DCNS.2020.22.1/macrocq [2] XU X, ZOU X B, LI T Y. Expert consensus on early identification, screening and early intervention of children with autism spectrum disorders[J]. Chin J Pediatr, 2017, 55(12): 890-897. [3] KIM Y S, LEVENTHAL B L, KOH Y J, et al. Prevalence of autism spectrum disorders in a total population sample[J]. Am J Psychiatry, 2011, 168(9): 904-912. doi: 10.1176/appi.ajp.2011.10101532 [4] BRODER-FINGERT S, BRAZAUSKAS K, LINDGREN K, et al. Pr-evalence of overweight and obesity in a large clinical sample of children with autism[J]. Acad Pediatr, 2014, 14(4): 408-414. doi: 10.1016/j.acap.2014.04.004 [5] WENTZ E, BJÖRK A, DAHLGREN J. Is There an overlap between eating disorders and neurodevelopmental disorders in children with obesity?[J]. Nutrients, 2019, 11(10): 2496. doi: 10.3390/nu11102496 [6] JACHYRA P, ANAGNOSTOU E, KNIBBE T J, et al. Weighty conversations: caregivers', children's, and clinicians' perspectives and experiences of discussing weight-related topics in healthcare consultations[J]. Autism Res, 2018, 11(11): 1500-1510. doi: 10.1002/aur.2017 [7] 李阳, 梁爽, 韩盼盼, 等. 孤独症谱系障碍儿童体成分病例对照研究[J]. 中国学校卫生, 2016, 37(6): 831-834. https://www.cnki.com.cn/Article/CJFDTOTAL-XIWS201606008.htmLI Y, LIANG S, HAN P P, et al. A case-control study on body composition of ASD children[J]. Chin J Sch Health, 2016, 37(6): 831-834. https://www.cnki.com.cn/Article/CJFDTOTAL-XIWS201606008.htm [8] BAUSET S M, ZAZPE I, SANCHIS A M, et al. Are there anthropometric differences between autistic and healthy children?[J]. J Child Neurol, 2013, 28(10): 1226-1232. doi: 10.1177/0883073812458832 [9] GARCIA-PASTOR T, SALINERO J J, THEIRS C I, et al. Obesity status and physical activity. level in children and adults with autism spectrum disorders: a pilot study[J]. J Autism Dev Disord, 2019, 49(1): 165-172. doi: 10.1007/s10803-018-3692-9 [10] RANJAN S, NASSER J A. Nutritional status of individuals with autism spectrum disorders: do we know enough?[J]. Adv Nutr, 2015, 6(4): 397-407. doi: 10.3945/an.114.007914 [11] ZHENG Z, ZHANG L, LI S, et al. Association among obesity, overweight and autism spectrum disorder: a systematic review and Meta-analysis[J]. Sci Rep, 2017, 7(1): 11697. doi: 10.1038/s41598-017-12003-4 [12] BARNHILL K, GUTIERREZ A, GHOSSAINY M, et al. Growth status of children with autism spectrum disorder: a case-control study[J]. J Hum Nutr Diet, 2017, 30(1): 59-65. doi: 10.1111/jhn.12396 [13] BICER A H, ALSAFFAR A A. Dietary intake and physical activity levels of male adolescents with autism spectrum disorder (ASD) and normal to high body mass index (BMI): a case series study[J]. Res Autism Spectrum Disord, 2016, 31(C): 1-10. [14] CASTRO K, FACCIOLI L S, BARONIO D, et al. Feeding behavior and dietary intake of male children and adolescents with autism spectrum disorder: a case-control study[J]. Int J Dev Neurosci, 2016, 53(C): 68-74. [15] HILL A P, ZUCKERMAN K E, FOMBONNE E. Obesity and Autism[J]. Pediatrics, 2015, 136(6): 1051-1061. doi: 10.1542/peds.2015-1437 [16] KUMMER A, BARBOSA I G, RODRIGUES D H, et al. Frequency of overweight and obesity in children and adolescents with autism and attention deficit/hyperactivity disorder[J]. Rev Paul Pediatr, 2016, 34(1): 71-77. doi: 10.1016/j.rpped.2015.06.013 [17] LIU X, LIU J, XIONG X Q, et al. Correlation between nutrition and symptoms: nutritional survey of children with autism spectrum Disorder in Chongqing, China[J]. Nutrients, 2016, 8(5): 294. doi: 10.3390/nu8050294 [18] PHILLIPS K L, SCHIEVE L A, VISSER S, et al. Prevalence and impact of unhealthy weight in a national sample of us adolescents with autism and other learning and behavioral disabilities[J]. Matern Child Health J, 2014, 18(8): 1964-1975. doi: 10.1007/s10995-014-1442-y [19] RIMMER J H, YAMAKI K, LOWRY B M, et al. Obesity and obesity-related secondary conditions in adolescents with intellectual/developmental disabilities[J]. J Intellect Disabil Res, 2010, 54(9): 787-794. doi: 10.1111/j.1365-2788.2010.01305.x [20] SHEDLOCK K, SUSI A, GORMAN G H, et al. Autism spectrum disorders and metabolic complications of obesity[J]. J Pediatr, 2016, 178: 183-187. doi: 10.1016/j.jpeds.2016.07.055 [21] LEVY S E, PINTO-MARTIN J A, BRADLEY C B, et al. Relationship of weight outcomes, co-occurring conditions, and severity of autism spectrum disorder in the study to explore early development[J]. J Pediatr, 2019, 205: 202-209. doi: 10.1016/j.jpeds.2018.09.003 [22] TWIG G, YANIV G, LEVINE H, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood[J]. N Engl J Med, 2016, 374: 2430-2440. doi: 10.1056/NEJMoa1503840 [23] LEE D H, KEUM N, HU F B, et al. Comparison of the association of predicted fat mass, body mass index, and other obesity indicators with type 2 diabetes risk: two large prospective studies in US men and women[J]. Eur J Epidemiol, 2018, 33: 1113-1123. doi: 10.1007/s10654-018-0433-5 [24] CAPUTI P, IVERSON D. Lack of sleep could increase obesity in children and too. much television could be partly to blame[J]. Acta Paediatr, 2014, 103(1): e27-31. doi: 10.1111/apa.12447 [25] HODGE D, CAROLLO T M, LEWIN M, et al. Sleep patterns in children with and without autism spectrum disorders: developmental comparisons[J]. Res Dev Disabil, 2014, 35(7): 1631-1638. doi: 10.1016/j.ridd.2014.03.037 [26] MATHESON B E, DRAHOTA A, BOUTELLE K N. A pilot study investigating the feasibility and acceptabilityof a parent-only behavioral weight-loss treatment for children with autism spectrum disorder[J]. J Autism Dev Disord, 2019, 49(11): 4488-4497. doi: 10.1007/s10803-019-04178-8 [27] KAMAL NOR N, GHOZALI A H, ISMAIL J. Prevalence of overweight and obesity among children and adolescents with autism spectrum disorder and associated risk factors[J]. Front Pediatr, 2019, 7: 38. doi: 10.3389/fped.2019.00038 [28] MUST A, ELIASZIW M, PHILLIPS S M, et al. The effect of age on the prevalence of obesity among US Youth with Autism spectrum disorder[J]. Child Obes, 2017, 13(1): 25-35. doi: 10.1089/chi.2016.0079 期刊类型引用(4)
1. 方美欣,何木叶,刘静怡,刘电芝. 孤独症青少年发展特点及干预进展研究综述. 现代特殊教育. 2025(06): 61-69 .  百度学术
百度学术2. 胡云扬,田耕畅,刘蒙,汪鸿. 孟德尔随机化研究在孤独症谱系障碍中的研究进展. 中国当代儿科杂志. 2024(05): 535-540 .  百度学术
百度学术3. 耿慧,傅涛. 孤独症谱系障碍儿童体育干预研究进展. 中国学校卫生. 2022(12): 1915-1920 .  本站查看
本站查看4. 邱明兰,吴慧娟,邓小军. 社会学视角下肥胖问题研究. 萍乡学院学报. 2022(06): 66-69+80 .  百度学术
百度学术其他类型引用(2)
-








 下载:
下载:
 下载:
下载:

