Effects of high temperature on children's emergency admissions during summer from 2016 to 2018 in Beijing
-
摘要:
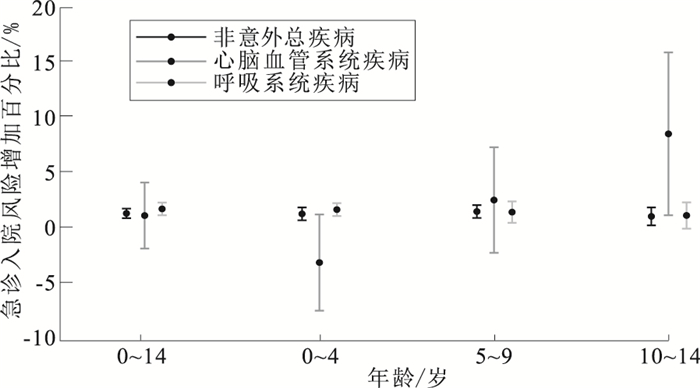
目的 分析北京市夏季高温对儿童急诊入院的不良影响,为儿童高温健康防护政策的制定提供科学依据。 方法 收集2016—2018年夏季(6—9月)北京市30家医院儿童急诊入院数据及同期逐日气象因素和空气污染物数据。基于Quasi-Possion回归广义线性模型分析北京市夏季日平均温度对儿童因非意外总疾病、心脑血管系统疾病、呼吸系统疾病急诊入院的影响。 结果 2016—2018年夏季,北京市日均温度为(24.06±3.59)℃,日相对湿度为(65.08±17.45)%。暴露当日日平均温度每升高1 ℃,北京市0~14岁儿童因非意外总疾病、呼吸系统疾病急诊入院风险分别增加0.21,0.64倍,尚未观察到高温对于儿童因心脑血管系统疾病急诊入院的影响。高温对于不同年龄组儿童急诊入院影响不一致,其中5~9岁儿童因非意外总疾病急诊入院风险增幅最大,0~4岁儿童易受呼吸系统疾病急诊入院的影响,10~14岁儿童受心脑血管系统疾病急诊入院影响最大。 结论 北京市夏季高温对儿童急诊入院具有显著影响,儿童呼吸系统疾病是夏季高温相关敏感性疾病,相关部门应该给予充分关注。 Abstract:Objective To explore the adverse effects of high temperature on emergency admissions of children during the summer in Beijing. Methods Child emergency admissions was collected from 30 hospitals in Beijing during the summer of 2016-2018, as well as data related to meteorological factors and air pollutant concentrations. A generalized linear model was used to analyze the association between the daily mean temperature and emergency admissions of children due to total non-accidental diseases, circulatory diseases, and respiratory diseases during the summer in Beijing. Results During the summer of 2016 to 2018 in Beijing, the daily mean temperature was (24.06±3.59)℃, and the daily mean relative humidity was (65.08±17.45)%. Every 1 ℃ increase in the daily mean temperature on the day of exposure had a significant effect on emergency admissions of children, aged 0-14 years old, due to total non-accidental diseases and respiratory diseases in Beijing, such that the risk of emergency admissions increased by 0.21, 0.64 times, respectively. The effect of high temperature on emergency admissions due to circulatory diseases was not significant. High temperature had inconsistent effects on emergency admissions of children from different age groups. Among them, the largest increase in the risk of emergency admissions due to total non-accidental diseases was observed among children aged 5-9 years old, while children aged 0-4 were vulnerable to emergency admissions for respiratory diseases, and emergency admissions for circulatory diseases were the highest among children aged 10-14. Conclusion High temperature had a significant effect on emergency admissions of children during the summer in Beijing. Pediatric respiratory diseases are sensitive diseases that are associated with a high temperature in summer, and greater attention should be given to this issue. -
Key words:
- Temperature /
- Humidity /
- Emergency treatment /
- Regression analysis /
- Child
-
表 1 北京市2016—2018年夏季lag0的日平均温度与0~14岁儿童急诊入院敏感性分析[急诊入院风险增加百分比(95%CI)/%]
Table 1. The sensitivity analysis of daily mean temperature at lag0 day and children aged 0-14 years old in the emergency department in summer from 2016 to 2018 in Beijing[the risk of emergency admission(95%CI)/%]
组别 自由度 非意外总疾病 心脑血管系统疾病 呼吸系统疾病 主模型 2 1.22(0.80~1.64) 0.99(-1.92~3.99) 1.64(1.09~2.20) 调整模型自由度 3 0.97(0.53~1.40) 0.81(-2.21~3.92) 1.35(0.78~1.93) 4 0.92(0.50~1.33) 0.87(-2.19~4.03) 1.28(0.74~1.82) 调整湿度为样条函数 2 1.22(0.80~1.64) 1.02(-1.89~4.01) 1.64(1.09~2.21) 注:调整了时间样条函数自由度和调整湿度为样条函数。 表 2 北京市2016—2018年夏季lag0的日平均温度与0~14岁儿童急诊入院敏感性分析[急诊入院风险增加百分比(95%CI)/%]
Table 2. The sensitivity analysis of daily mean temperature at lag0 day and children aged 0-14 years old in the emergency department in summer from 2016 to 2018 in Beijing[the risk of emergency admission(95%CI)/%]
模型 变量 非意外总疾病 心脑血管系统疾病 呼吸系统疾病 主模型加入PM2.5调整模型(dftime=2) 日平均温度(每变化1 ℃) 0.97(0.48~1.46) 1.83(-1.59~5.37) 1.36(0.71~2.01) PM2.5(每变化10 μg/m3) 0.04(-0.00~0.08) -0.12(-0.39~0.14) 0.04(-0.01~0.09) 主模型加入O3调整模型(dftime=2) 日平均温度(每变化1 ℃) 1.18(0.64~1.72) -0.16(-3.86~3.69) 1.65(0.93~2.38) O3(每变化10 μg/m3) 0.05(-0.36~0.46) 1.41(-1.50~4.41) -0.01(-0.56~0.54) 注:模型中加入空气污染物。 -
[1] Intergovernmental Panel on Climate Change. Climate change 2014: synthesis report[EB/OL]. [2020-11-29]. https://archive.ipcc.ch/report/ar5/syr. [2] World Meteorological Organization. WMO Statement on the state of the global climate in 2019[EB/OL]. [2020-11-29]. https://library.wmo.int. [3] BASU R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008[J]. Environ Health, 2009, 8(1): 1-13. doi: 10.1186/1476-069X-8-1 [4] ZHANG H, LIU S, CHEN Z, et al. Effects of variations in meteorological factors on daily hospital visits for asthma: a time-series study[J]. Environ Res, 2020, 182: 109115-109121. doi: 10.1016/j.envres.2020.109115 [5] PAOLA M, GABRIELE A, MANUELA D S. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities[J]. Am J Respir Crit Care Med, 2009, 179(5): 383-389. doi: 10.1164/rccm.200802-217OC [6] PHUNG D, THAI P K, GUO Y, et al. Ambient temperature and risk of cardiovascular hospitalization: an updated systematic review and meta-analysis[J]. Sci Total Environ, 2016, 550: 1084-1102. doi: 10.1016/j.scitotenv.2016.01.154 [7] GRONLUND C J, SULLIVAN K P, KEFELEGN Y, et al. Climate change and temperature extremes: a review of heat-and cold-related morbidity and mortality concerns of municipalities[J]. Other, 2018, 114: 54-59. http://www.ncbi.nlm.nih.gov/pubmed/29907247 [8] LIN Y K, SUNG F C, HONDA Y, et al. Comparative assessments of mortality from and morbidity of circulatory diseases in association with extreme temperatures[J]. Sci Total Environ, 2020, 723: 138012. doi: 10.1016/j.scitotenv.2020.138012 [9] VAN LOENHOUT J A F, DELBISO T D, KIRILIOUK A, et al. Heat and emergency room admissions in the Netherlands[J]. BMC Public Health, 2018, 18(1): 108. doi: 10.1186/s12889-017-5021-1 [10] BAI L, CIRENDUNZHU, WOODWARD A, et al. Temperature, hospital admissions and emergency room visits in Lhasa, Tibet: a time-series analysis[J]. Sci Total Environ, 2014, 490: 838-848. doi: 10.1016/j.scitotenv.2014.05.024 [11] ANDERSON G B, DOMINICI F, WANG Y, et al. Heat-related emergency hospitalizations for respiratory diseases in the medicare population[J]. Am J Resp Crit Care Med, 2013, 187(10): 1098-1103. doi: 10.1164/rccm.201211-1969OC [12] OKTAY C, LUK H J, ALLEGRA J R, et al. The effect of temperature on illness severity in emergency department congestive heart failure patients[J]. Annals Acad Med, 2009, 38(12): 1081-1084. http://www.sciencedirect.com/science/article/pii/S019606440700978X [13] ZHANG Y, YAN C, KAN H, et al. Effect of ambient temperature on emergency department visits in Shanghai, China: a time series study[J]. Environ Health, 2014, 13(1): 100-108. doi: 10.1186/1476-069X-13-100 [14] WANG X Y, BARNETT A G, YU W, et al. The impact of heatwaves on mortality and emergency hospital admissions from non-external causes in Brisbane, Australia[J]. Occup Environ Med, 2012, 69(3): 163-169. doi: 10.1136/oem.2010.062141 [15] Intergovernmental Panel on Climate Change. Global warming of 1.5 ℃[EB/OL]. [2020-11-29]. https://www.ipcc.ch/sy15. [16] KNOWLTON K, ROTKIN-ELLMAN M, KING G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits[J]. Environ Health Perspect, 2009, 117(1): 61-67. doi: 10.1289/ehp.11594 [17] BUNYAVANICH S, LANDRIGAN C P, MCMICHAEL A J, et al. The impact of climate change on child health[J]. Ambulat Pediatr, 2003, 3(1): 44-52. doi: 10.1367/1539-4409(2003)003<0044:TIOCCO>2.0.CO;2 [18] XU Z, ETZEL R A, SU H, et al. Impact of ambient temperature on children's health: a systematic review[J]. Environ Res, 2012, 117: 120-131. doi: 10.1016/j.envres.2012.07.002 [19] EBI K L, PAULSON J A. Climate change and child health in the united states[J]. Curr Problems Pediatr Adolesc Health Care, 2010, 40(1): 2-18. doi: 10.1016/j.cppeds.2009.12.001 [20] KOVATS R S, HAJAT S, WILKINSON P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK[J]. Occup Environ Med, 2004, 61(11): 893-898. doi: 10.1136/oem.2003.012047 [21] XU Z, HU W, SU H, et al. Extreme temperatures and paediatric emergency department admissions[J]. J Epidemiol Commun Health, 2014, 68(4): 304-311. doi: 10.1136/jech-2013-202725 [22] National Weather Service. Vapor pressure calculator[EB/OL]. [2020-11-30]. https://www.weather.gov/media/epz/wxcalc/vaporPressure.pdf. [23] NITSCHKE M, TUCKER G R, HANSEN A L, et al. Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: a case-series analysis[J]. Environ Health, 2011, 10(1): 42-51. doi: 10.1186/1476-069X-10-42 [24] PIOTR W, ANNA G, ALANA M, et al. Extreme heat and paediatric emergency department visits in Southwestern Ontario[J]. Paediatr Child Health, 2020, pxaa096: 1-8. DOI: 10.1093/pch/pxaa096. [25] PRIFTIS K N, PALIATSOS A G, PANAGIOTOPOULOU-GARTAGANI P, et al. Association of weather conditions with childhood admissions for wheezy bronchitis or asthma in Athens[J]. Respiration, 2006, 73(6): 783-790. doi: 10.1159/000093817 [26] BLUM L N, BRESOLIN L B, WILLIAMS M A. Heat-related illness during extreme weather emergencies[J]. JAMA, 1998, 279(19): 1514. doi: 10.1001/jama.279.19.1514 [27] SHEFFIELD P E, LANDRIGAN P J. Global climate change and children's health: threats and strategies for prevention[J]. Environ Health Perspect, 2011, 119(3): 291-298. doi: 10.1289/ehp.1002233 [28] GUO W F, YI L, WANG P, et al. Assessing the effects of meteorological factors on daily children's respiratory disease hospitalizations: a retrospective study[J]. Heliyon, 2020, 6(8): e04657. doi: 10.1016/j.heliyon.2020.e04657 [29] ROCHELLE G, RUPA B, BRAIN M, et al. The effect of temperature on hospital admissions in nine California counties[J]. Int J Public Health, 2010, 55(2): 113-121. doi: 10.1007/s00038-009-0076-0 [30] XU Z, HU W, TONG S. Temperature variability and childhood pneumonia: an ecological study[J]. Environ Health, 2014, 13(1): 51. doi: 10.1186/1476-069X-13-51 [31] PUDPONG N, HAJAT S. High temperature effects on out-patient visits and hospital admissions in Chiang Mai, Thailand[J]. Sci Total Environ, 2011, 409(24): 5260-5267. doi: 10.1016/j.scitotenv.2011.09.005 [32] IÑIGUEZ C, SCHIFANO P, ASTA F, et al. Temperature in summer and children's hospitalizations in two Mediterranean cities[J]. Environ Res, 2016, 150: 236-244. doi: 10.1016/j.envres.2016.06.007 -







 下载:
下载: